2.3 Posterior Segment Differential Diagnoses and Aetiologies
When describing differential diagnoses, try to categorise your list into either:
- Most common first
- Most serious first
- Pathological sub-groups (e.g. infection, neoplasia etc.)
- Angioid Streaks
- Bull’s Eye Maculopathy
- Choroidal Folds
- Choroidal Tumour
- Choroidal Neovascularisation
- Cotton Wool Spots
- Crystalline Retinopathy
- Cherry Red Spot
- Cystoid Macular Oedema
- Deafness
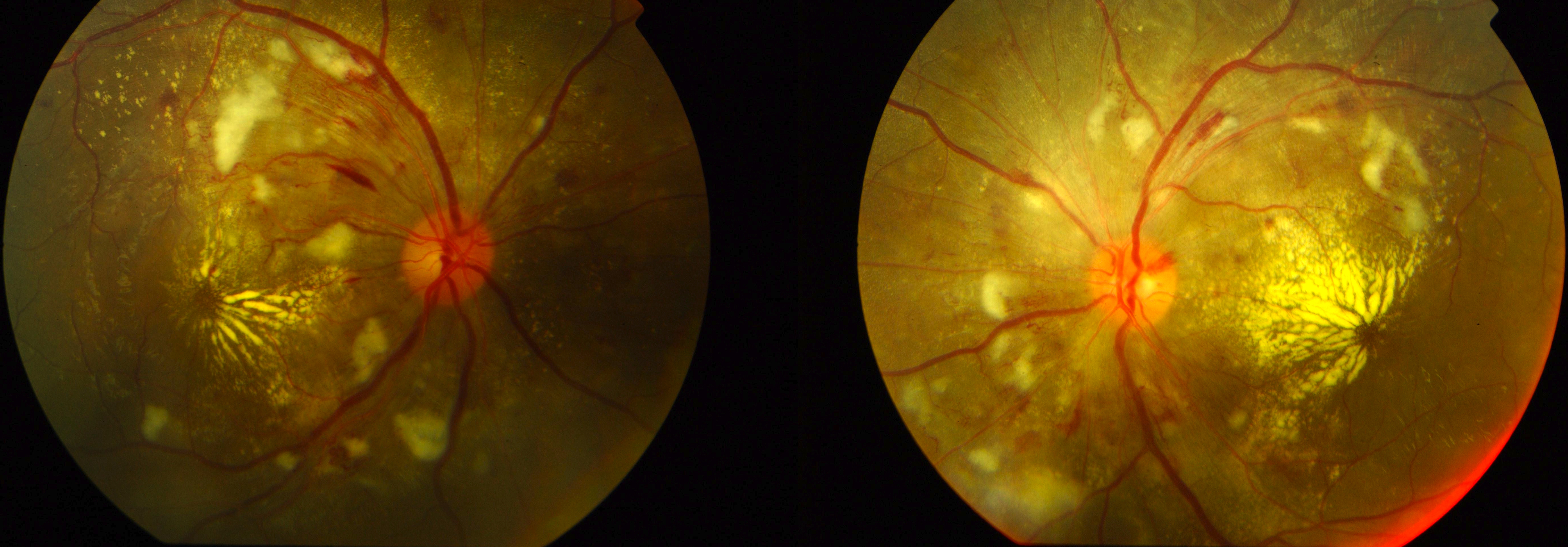
- Diabetic Retinopathy
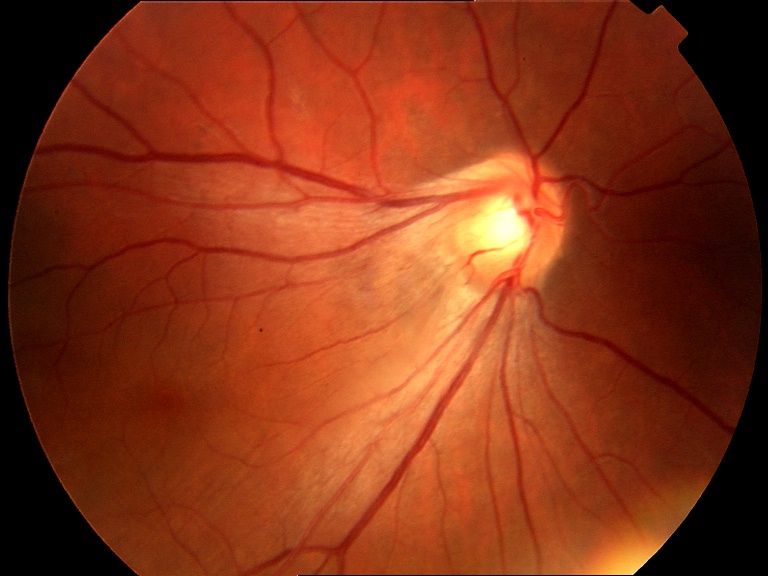
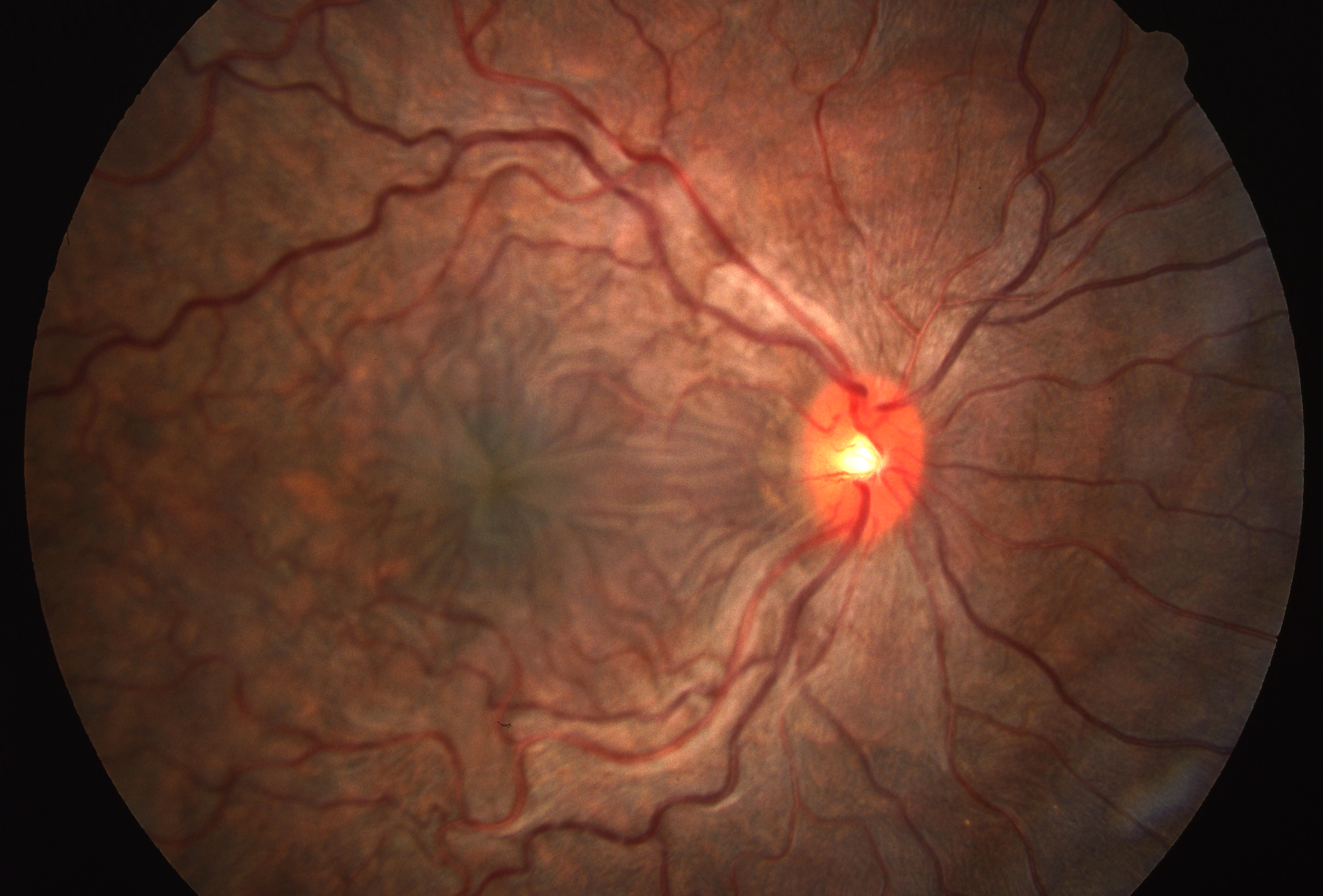
- Dragged Optic Disc
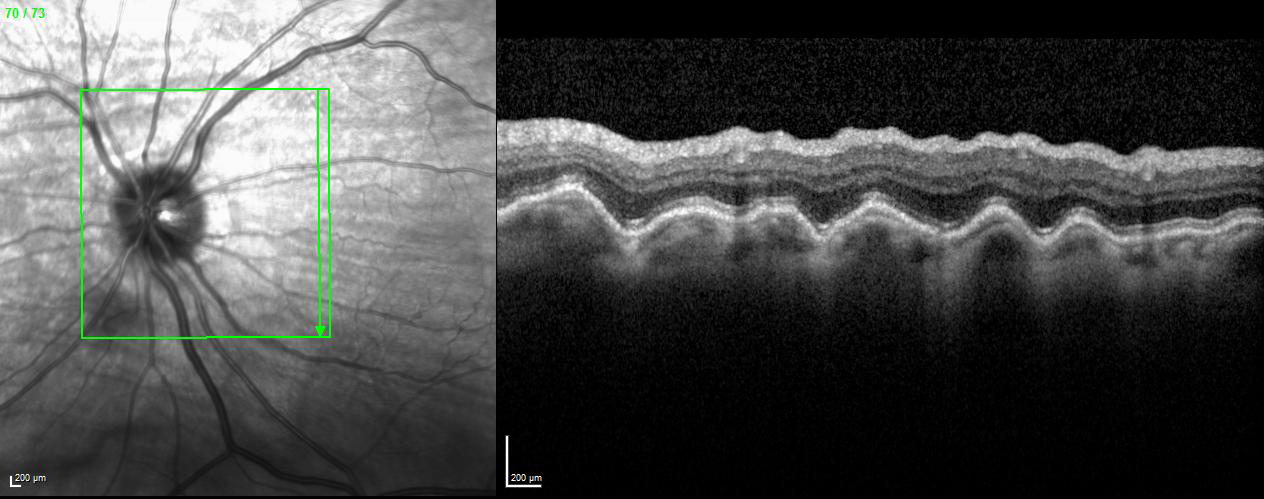
- Epiretinal Membrane
- Normal Fundus with Decreased Vision (Masqueraders of Functional Vision Loss)
- Pigmentary Retinopathy
- Retinal Artery Occlusions
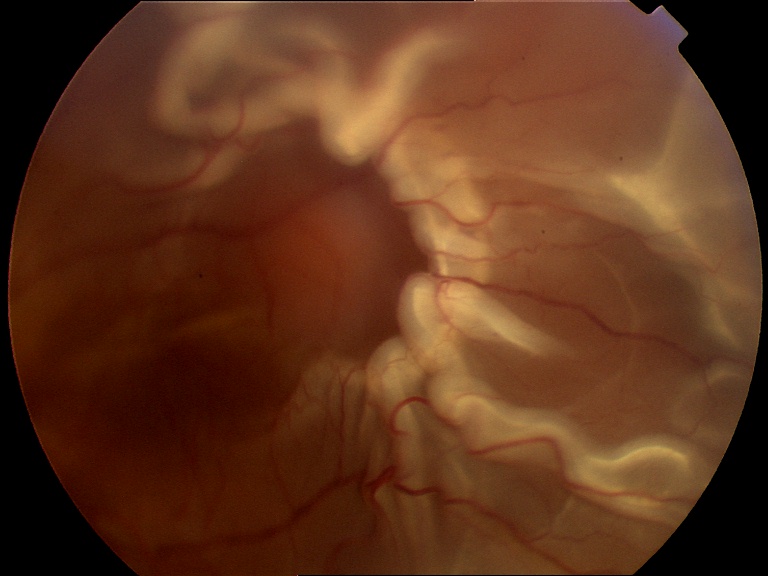
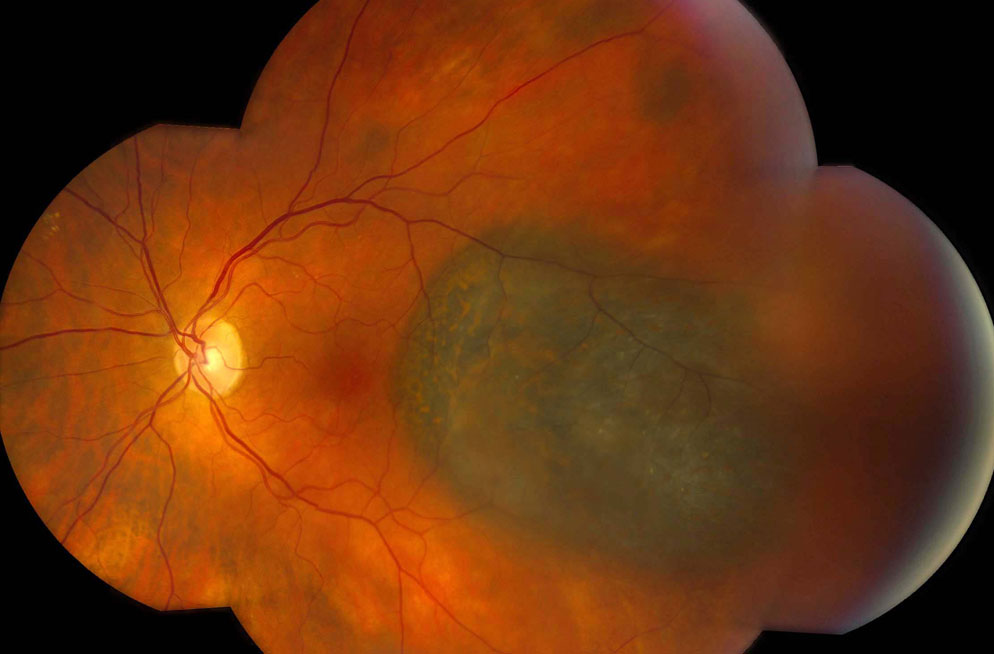
- Retinal Detachment (Rhegmatogenous)
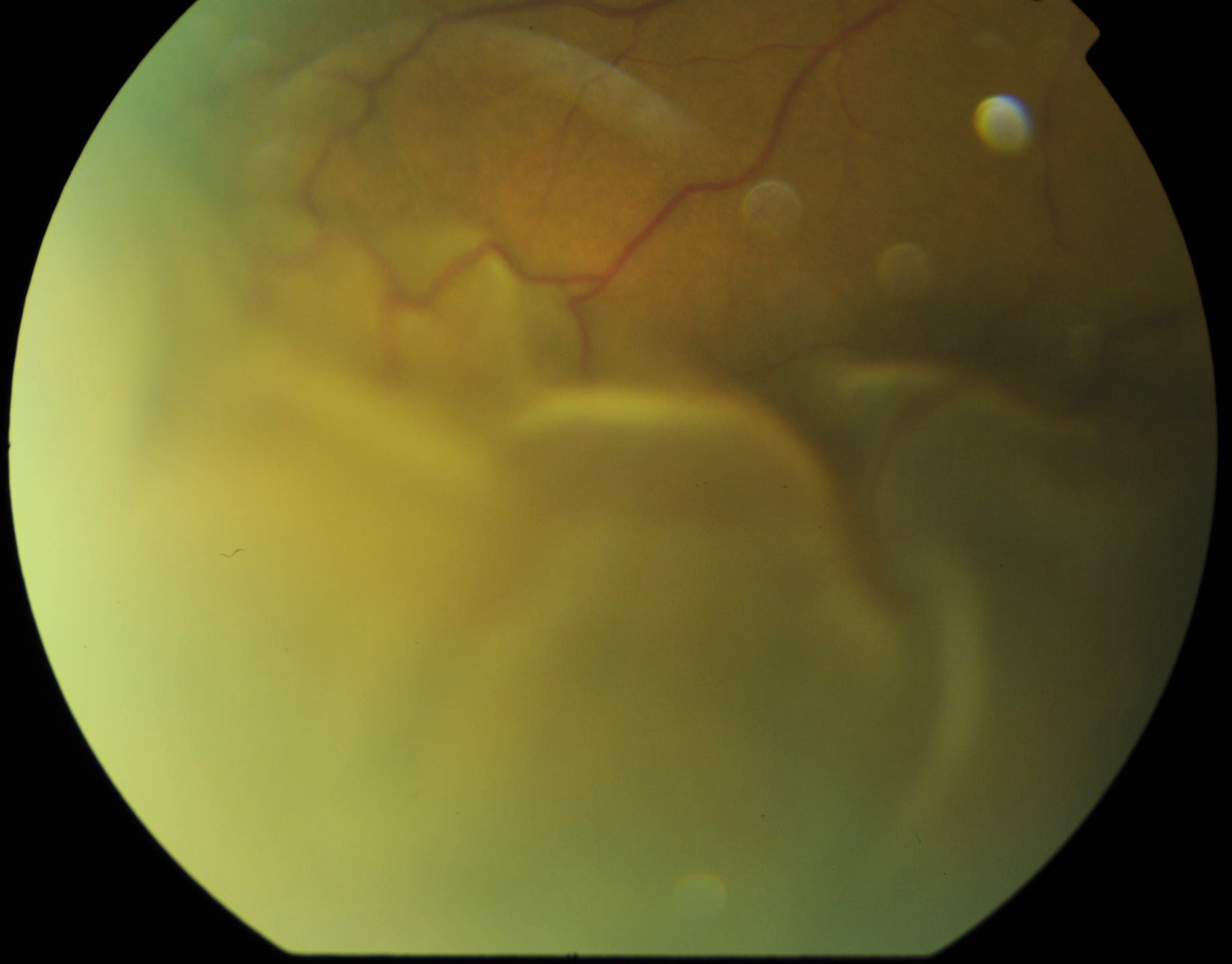
- Retinal Detachment (Exudative)
- Retinal Detachment (Tractional)
- Retinal Flecks
- Retinal Haemorrhages (in four quadrants)
- Retinal Haemorrhages (Multi-layered)
- Retinal Neovascularisation
- Retinal Vasculitis (See Chapter 4.0 – Uveitis)
- Retinal Vein Occlusions
- Submacular Haemorrhage
- Tumour (Fundus)
- Vitreous Haemorrhage
“PEPSI-MAX”
- P seudoxanthomaelasticum
- E hlers-Danlos type 6
- P aget’s, Acromegaly
- S ickle cell, Thalassaemia
- I diopathic (50% of angioid streaks)
- M yopia
- A cromegaly, Abetalipoproteinaemia
- To X ic (Lead poisoning)
“If you know your ABC’s then you’re a STAR!”
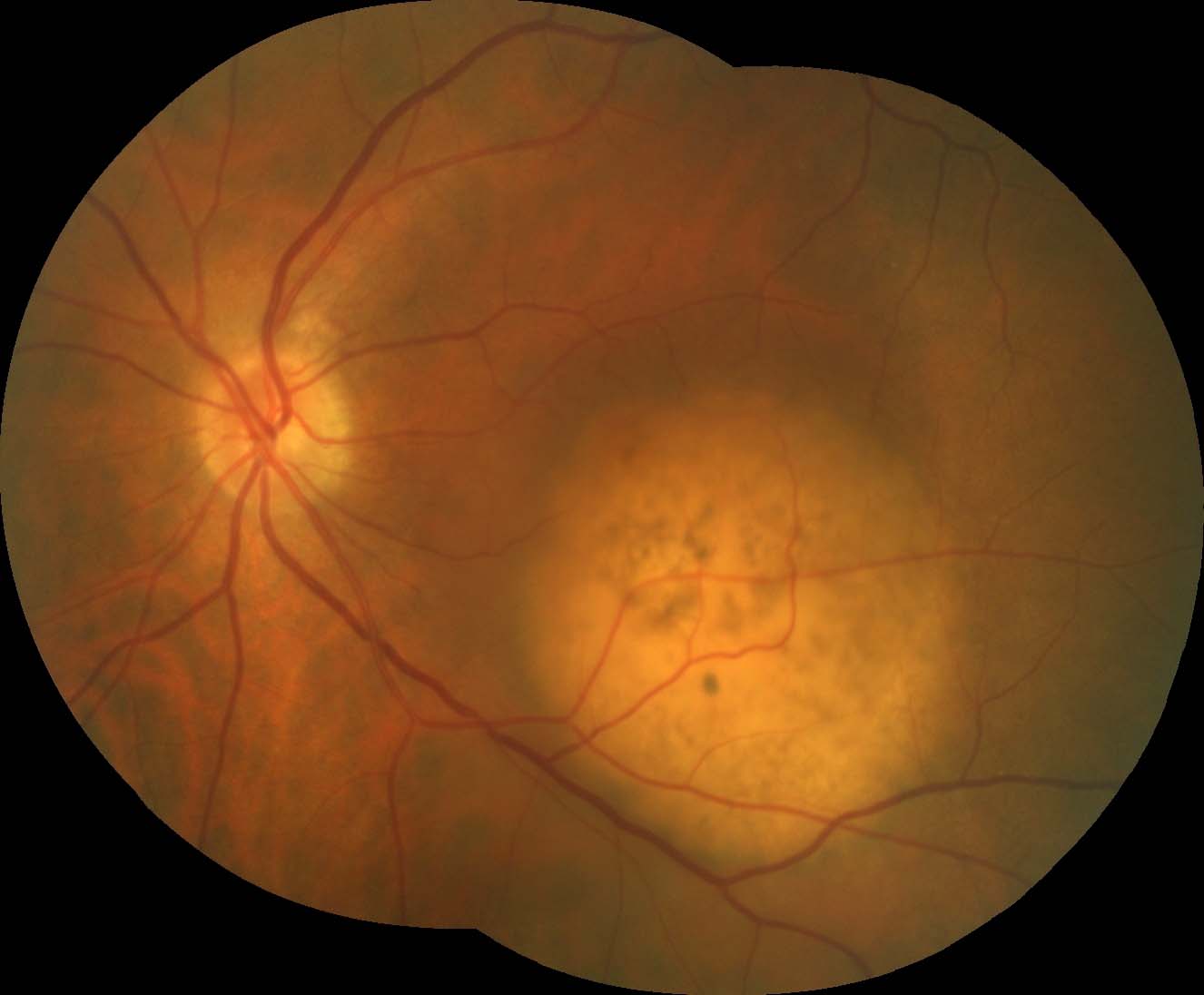
- A MD, A nnular Dystrophy
- B atten disease, B enign concentric annular macular dystrophy
- C hloroquine / Hydroxychloroquine, C one dystrophy
- STAR gardt
Within Eye
- Idiopathic
- Hypermetropia
- Hypotony
- AMD
- Posterior scleritis
- Choroidal tumours
- Papilloedema / ↑ICP
Outside Eye
- Orbital tumours
- Scleral buckle
- IOID
- TED
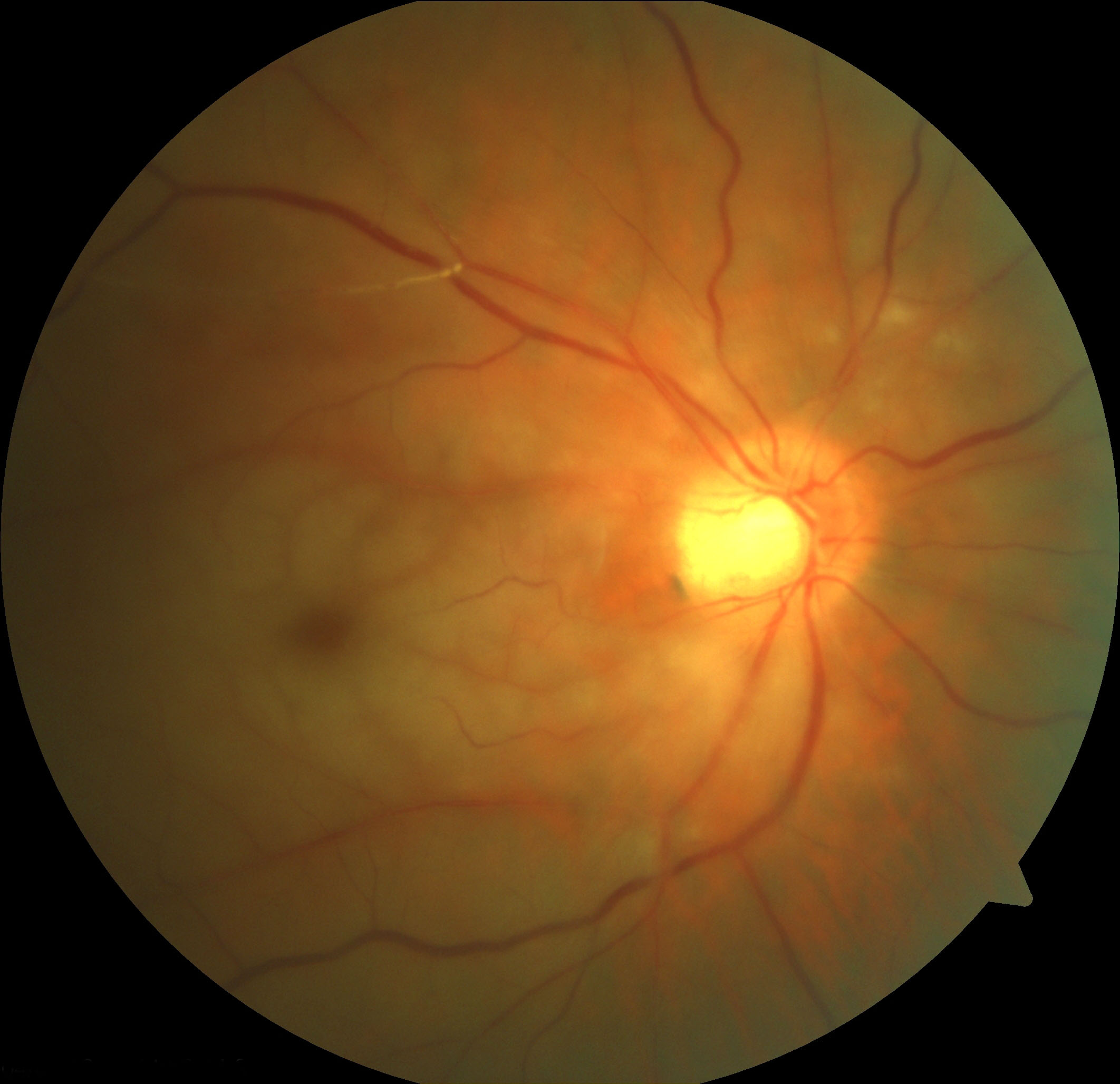
Pigmented
Non-pigmented
Non-Malignant
Pigmented
Naevus
(NB: haemorrhage can masquerade as pigmentation)
Non-pigmented
- Amelanotic naevus
- Choroidal haemangioma
- Choroidal osteoma
- Granuloma (TB, Sarcoidosis
Malignant
Pigmented
Melanoma
Non-pigmented
- Amelanotic melanoma
- Metastasis
- Lymphoma (but may have leopard spotting)
Degenerative
AMD / PCV, Myopia, Angioid streaks
Uveitis
Posterior uveitis (MFC / PIC, POHS)
Trauma
Choroidal rupture, heavy laser
Tumours
Choroidal nevi, osteoma
Idiopathic
CNV Sub-type:
- Type 1: Sub-RPE, most AMD
- Correlates with occult CNV on fluorescein angiogram
- Type 2: Sub-retinal, most non-AMD
- Correlates with classic CNV on fluorescein angiogram
- Type 3: Intra-retinal (e.g. RAP)
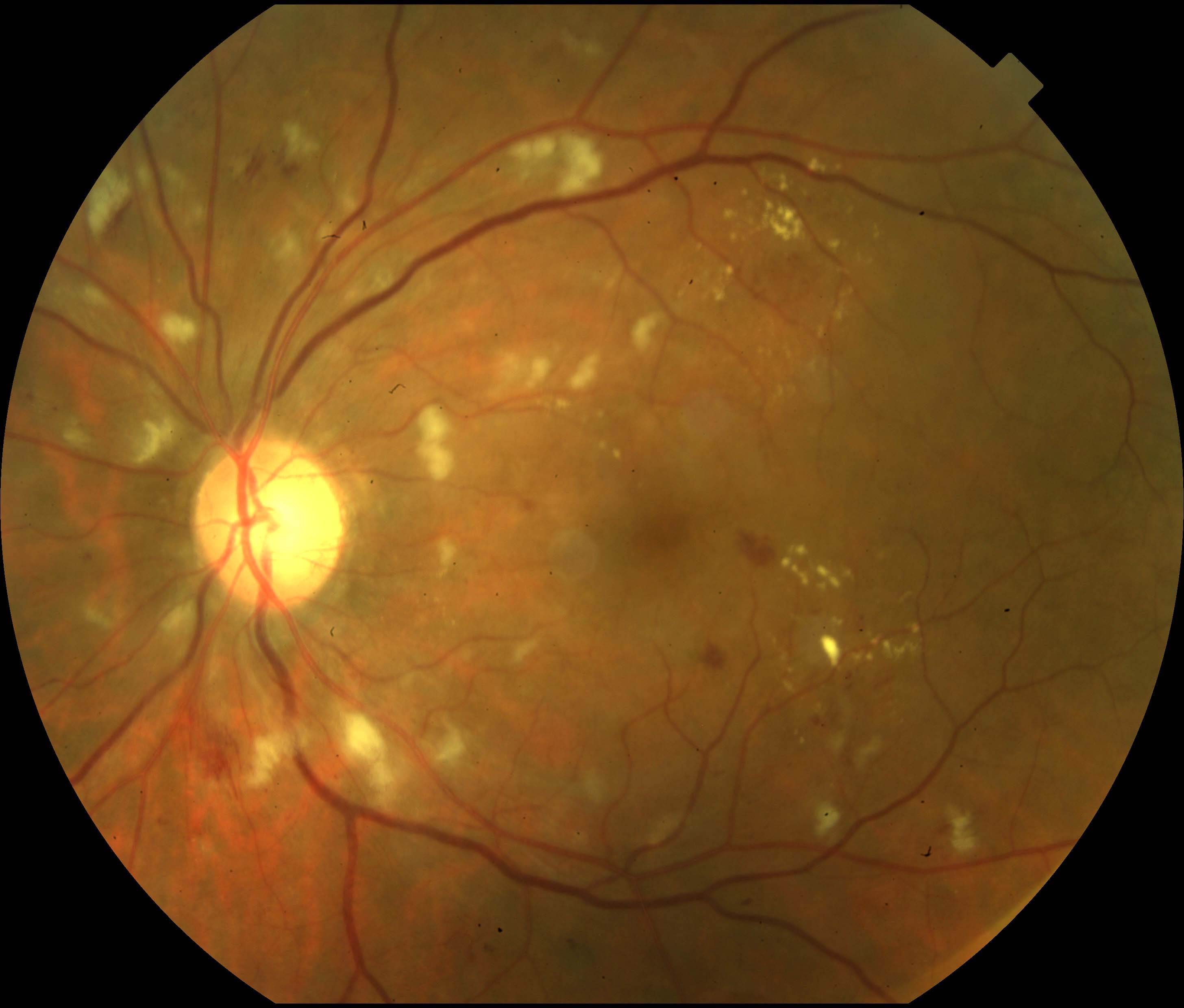
Vascular
Diabetes, HT, RVO,OIS, anaemia, hyperviscosity, radiation, emboli
Inflammatory
SLE
Infectious
HIV Retinopathy
Neoplastic
Leukaemia
Medication
Interferon retinopathy
Miscellaneous
Purtscher, High-altitude retinopathy, Idiopathic
“(A)BCD-MS”
- (A lport syndrome- flecks, not true crystals)
- **B ietti crystalline dystrophy (AR or X-linked)
- Chronic retinal detachment**, Cystinosis / (Oxalosis), Calcified drusen
- Drugs: Triamcinolone, Tamoxifen, Tanning agent (Canthaxanthine), Talc, Nitrofurantoin
- M acular Telangiectasia type 2
- S jogren-Larson syndrome
- Central Retinal Artery Occlusion
- Commotio retinae
- Metabolic storage disease (e.g. Tay Sach’s Disease)
- Drug Toxicity (Quinine, Dapsone, Carbon monoxide, Methanol toxicity)
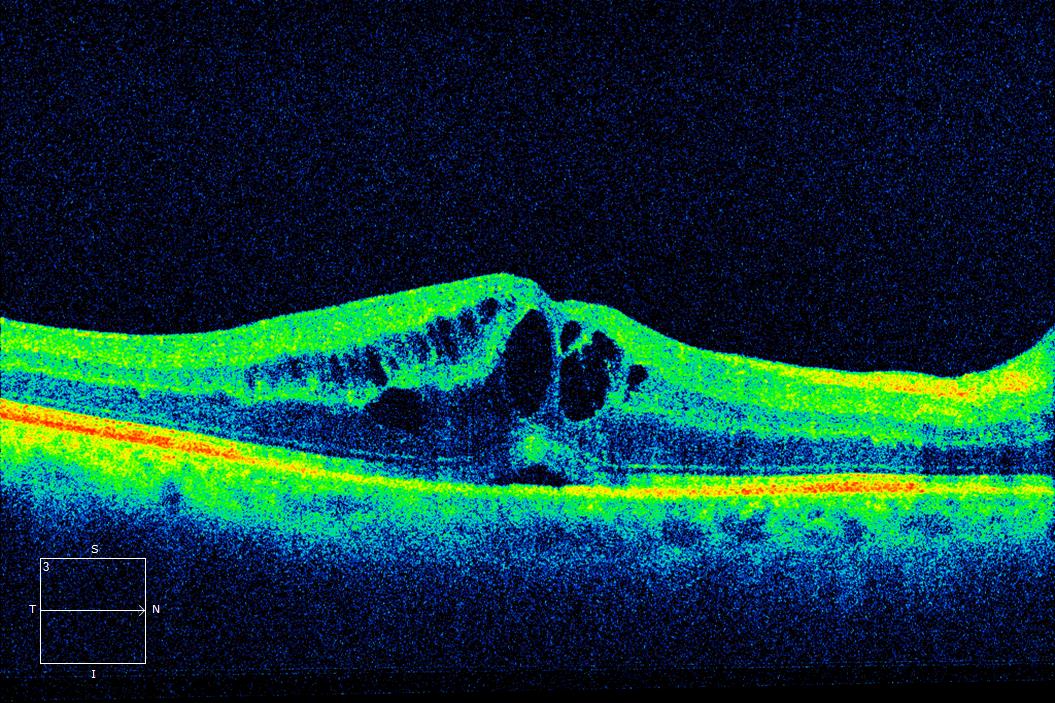
Vascular
Diabetes, HT, RVO, OIS, Macular Telangiectasia
Uveitis
Post-operative
AMD / CNV
Retinal Dystrophy
Retinitis Pigmentosa
Traction
ERM, VMT
Tumours
Choroidal haemangioma, Retinal capillary haemangioma
Systemic
Leukaemia
Drugs
Fingolimod
Dystrophies
Usher’s, Stickler’s, LCA, Albinism, MIDD, Alport’s, Norrie’s disease
Congenital
Syphilis, Rubella, CMV, Wolfram syndrome (DIDMOAD), Cystinosis
Uveitic
VKH, Susac’s, Cogan’s
Differential Diagnosis:
- Hypertensive retinopathy
- Retinal vein occlusion
- Ocular ischaemic syndrome
- Radiation retinopathy
- Macular telangiectasia type 1
- Sickle cell retinopathy
- ROP, FEVR, Norrie
- Toxocara
- Combined hamartoma of the retina and retinal pigment epithelium
- Incontinentia pigmenti
- Idiopathic
- Uveitis
- Retinal break, RD (laser / cryotherapy, retinal surgery)
- Retinal vascular disease (diabetes, RVO)
- CNV
- Neurofibromatosis
Younger patient:
- Refractive error
- Amblyopia
- Keratoconus
- Stargardt’s
- MEWDS
- Retrobulbar optic neuritis
Older patient:
Refractive
Amblyopia
Cornea
Keratoconus
Fundus
Stargardt’s, MEWDS, cone dystrophy, AZOOR, CAR / MAR, OIS (with featureless fundus)
Optic Nerve
Retrobulbar optic neuritis, PION, optic atrophy
Pituitary Apoplexy
Cortical
Cortical Visual Impairment (e.g. VVAD, CJD)
Functional Vision Loss
Hereditary
Retinitis pigmentosa (rod-cone dystrophies)
Uveitic
CMV Retinitis, Rubella, Syphilis (old)
Vascular
RVO (old)
Chronic Epithelial Detachment
Stargardt’s, MEWDS, cone dystrophy, AZOOR, CAR / MAR, OIS (with featureless fundus)
Trauma
Commotio (old), Intense PRP
Drugs
Chloroquine / Phenothiazines
Malignancy
CAR / MAR
Risk factors:
Age (older), males
Atherosclerosis
HT, Hypercholesterolaemia, diabetes, smoking, elderly
GCA
Commotio (old), Intense PRP
Peri-arteritis
SLE / Dermatomyositis, PAN / Wegener, Behçhet, Syphilis
Hyperviscosity
Polycythaemia, Multiple Myeloma, Waldenstrom Macroglobulinaemia
Thrombophilias
Drugs
Oral contraceptive pill
Retinal Migraine
Susac Syndrome
= BRAO, Deafness, Encephalopathy
- Retinoschisis
- Choroidal detachment
- Uveal Effusion Syndrome
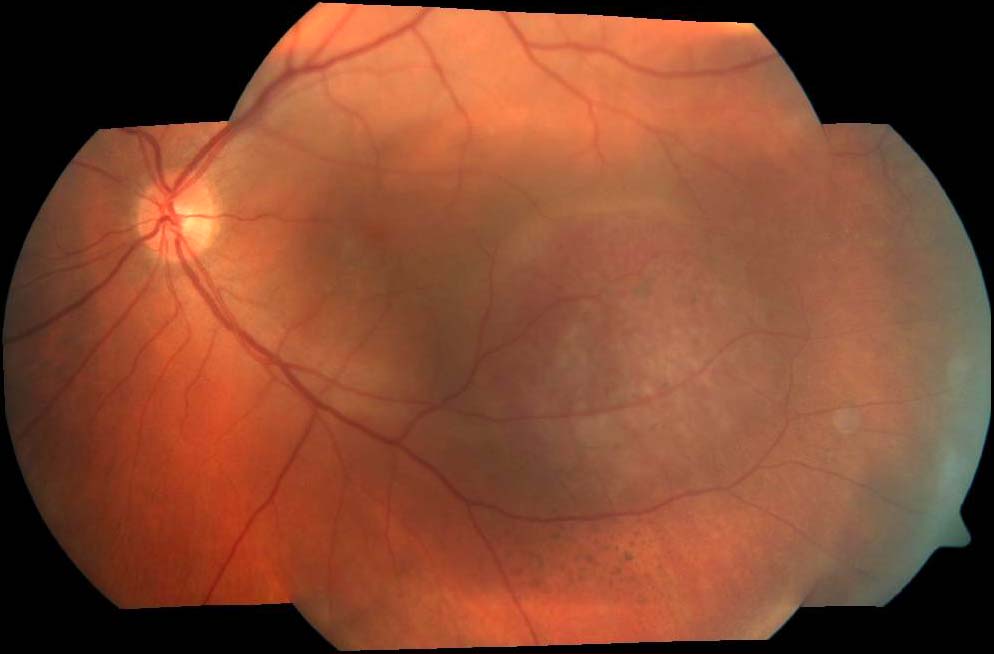
Macular Disorders
Central serous chorioretinopathy, AMD
Retinal Vascular Disease
Malignant hypertension, Coat’s disease
Uveitis / Posterior Scleritis
VKH, Sympathetic ophthalmia
Intra-ocular Tumours
Melanoma, Metastasis, Choroidal haemangioma, Retinal capillary haemangioblastoma
Optic Nerve
Optic Disc Pit
Systemic
(Pre)eclampsia, Hypoproteinaemia
Previous
2.2 Fundus Tumours
All rights reserved. No part of this publication which includes all images and diagrams may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the authors, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law.
Vitreoretinal Surgery Online
This open-source textbook provides step-by-step instructions for the full spectrum of vitreoretinal surgical procedures. An international collaboration from over 90 authors worldwide, this text is rich in high quality videos and illustrations.

.jpg)

.jpg)