7 Neuro-Ophthalmology
7.1 Cranial Nerve III (Oculomotor) Palsy
7.2 Cranial Nerve IV (Trochlear) Palsy
7.3 Cranial Nerve VI (Abducens) Palsy
7.4 Cranial Nerve VII (Facial) Palsy
7.5 Optic Nerve Function
7.6 Visual Fields to Confrontation
7.7 Pupils
7.8 Horner’s Syndrome
7.9 Nystagmus
7.10 Neuro-Ophthalmic Differential Diagnoses and Aetiologies
7.8 Horner's Syndrome
A Horner’s syndrome arises from pathology in the sympathetic innervation of the eye. The two main clinical features are anisocoria and ptosis- the candidate may be directed to examine pupils or eyelids, although it is more common to request the pupillary examination. Once a Horner’s syndrome is diagnosed, associated signs should be sought that will assist with localising the lesion (to central, pre-ganglionic and post-ganglionic).
1. Central
- Hypothalamus → Ciliospinal centre of Budge (C8-T2)
- Brainstem CVA (e.g. Lateral medullary syndrome), tumour, MS
- Cervical Syringomyelia
2. Pre-ganglionic
- Ciliospinal centre of Budge (C8-T2) → Superior cervical ganglion
- Cervical sympathectomy
- Thyroid cancer
- Pancoast tumour
3. Post-ganglionic
- Superior cervical ganglion → Eye
- Internal carotid artery dissection
- Cavernous sinus syndrome
4. Paediatric Horner’s
- Cardiac (VSD), Birth trauma, Neuroblastoma
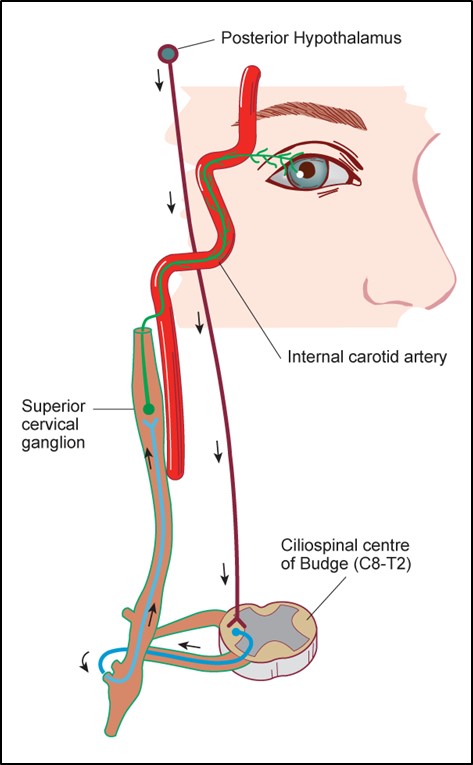
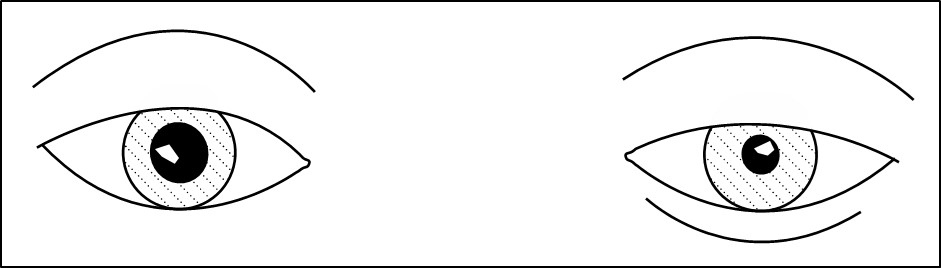
Figure 7.8.1
Oculo-sympathetic Pathway
A Horner’s Syndrome may be central (red), pre-ganglionic (blue) or post-ganglionic (green).
“Please examine this patient’s pupils”
Section 7.7 Pupils should be read in conjunction with this page.
i. Pupil Size (Anisocoria)
ii. Pupil Shape
iii. Heterochromia Iridis
- The affected side is lighter. Only present in congenital or early acquired Horner’s syndrome. If present in an adult with incidentally noted Horner’s Syndrome, further investigation for sinister neurological causes is unnecessary
iv. Eyelids
- Ptosis (paralysis of Müllers muscle)
- Inverse ptosis (lower lid elevation in Horner’s)
v. Strabismus (CNIII palsy)
Scars (neck scar with Horner’s, tracheostomy scar with previous trauma)
- Anisocoria worse in dark = Problem with the smaller pupil (not dilating)
- It is important to measure the pupils quickly once the room lights have been turned off. Patients with Horner’s syndrome have a dilatation lag - the affected pupil will dilate, but more slowly by passive relaxation of the sphincter pupillae alone (compared to the fellow eye with intact dilator pupillae activity)
- Normal pupillary light reflexes
- No RAPD
1. Anhidrosis
- Found only in central / preganglionic lesions proximal to the carotid artery bifurcation since sweat glands are supplied by external carotid artery sympathetics)
2. Neck
- Palpate in supraclavicular fossa, and check thyroid gland while asking patient to swallow, and look for scars
- Scar (Cervical sympathectomy)
- Thyroid cancer
- Supraclavicular lymphadenopathy (Pancoast tumour)
3. Hands
- Wasting / weakness (T1) – check for finger abduction by asking the patient to fan out their fingers against resistance
- Clubbing (Pancoast tumour), claw (Cervical cord)
4. Eye Movements
Check carefully for an ipsilateral minor abduction weakness or slowed abducting saccade CV VI (cavernous sinus)
5. Auscultate
- Carotid bruit? (Internal carotid artery dissection)
- Respiratory exam (Pancoast tumour)
6. Other Neurological Signs
- Brainstem CVA (e.g. Lateral medullary syndrome), tumour, MS, Cavernous sinus syndrome
- Ipsilateral hemisensory loss pain / temperature (Lateral medullary syndrome)
- Ask the patient to say “Ah!” and check gag reflex CN IX (Lateral medullary syndrome)
Limb Exam
- Contralateral hemisensory loss pain / temperature (Lateral medullary syndrome)
- Past pointing, Ataxia (Lateral medullary syndrome)
Speech
- Ask the patient to say “British Constitution”
- Hoarse? CN X Recurrent laryngeal nerve palsy (Pancoast tumour)
- Cerebellar dysarthria? (Lateral medullary syndrome)
7. Check Old Photos to See if the Horner’s Syndrome is Acute
- This is less commonly performed now since imaging (CT chest, MRI / MRA brain / neck) can localise most lesions. However it is important to be familiar with these techniques as they are still used in difficult cases. This area remains a common examination topic
Classical
Alternative
Diagnosis
Classical
Cocaine 10%
Will NOT dilate Horner’s
Alternative
Apraclonidine 1%
Will ABNORMALLY dilate Horner’s
Previous
7.7 Pupils
Next
7.9 Nystagmus
All rights reserved. No part of this publication which includes all images and diagrams may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the authors, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law.
Vitreoretinal Surgery Online
This open-source textbook provides step-by-step instructions for the full spectrum of vitreoretinal surgical procedures. An international collaboration from over 90 authors worldwide, this text is rich in high quality videos and illustrations.