7 Neuro-Ophthalmology
7.1 Cranial Nerve III (Oculomotor) Palsy
7.2 Cranial Nerve IV (Trochlear) Palsy
7.3 Cranial Nerve VI (Abducens) Palsy
7.4 Cranial Nerve VII (Facial) Palsy
7.5 Optic Nerve Function
7.6 Visual Fields to Confrontation
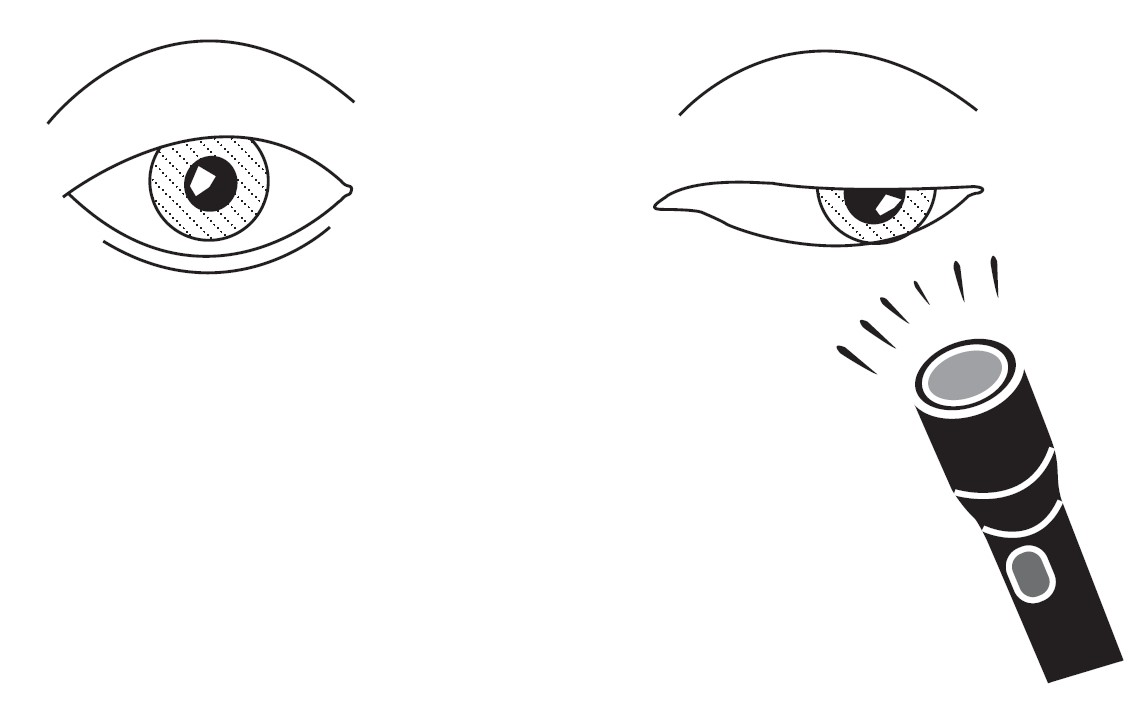
7.7 Pupils
7.8 Horner’s Syndrome
7.9 Nystagmus
7.10 Neuro-Ophthalmic Differential Diagnoses and Aetiologies
7.1 Cranial Nerve III (Oculomotor) Palsy
Cranial nerve III palsies may be associated with potentially life-threatening conditions - GCA, cerebral aneurysm, pituitary apoplexy - although these are generally not found in person in exams! However, these cases may be given as vignettes so it is important to be familiar with them. Most importantly, the examiner is looking for you to demonstrate that you can exclude these conditions. It is essential that the candidate look carefully for signs of a “surgical” cause - the pupillary exam is crucial.
- Abnormal head position - head turn to the opposite side
- Hirschberg (pupil margin = 30Δ, limbus = 90Δ) - eye “down and out”
- Ptosis = paralysis of levator (complete unilateral ptosis is almost always a CNIII palsy)
- ± Mydriasis = unopposed sympathetics (only occurs with “surgical” causes)
- Exotropia (greater on head turn to same side (i.e. incomitant)
- Hypotropia
- Lift the ptotic lid except when looking for aberrant regeneration
- Limitation of movement in all directions of gaze except laterally
+ Aberrant Regeneration?
+ CNIV Palsy?
NB: If all that is seen in failure of adduction, this might be an INO instead of a CNIII – so look for abducting nystagmus of the contralateral eye.
- Slow adducting, elevating
- Mydriasis (poor light response), with anisocoria worse in light
- Only occurs with “surgical” causes (that compress intra-neural papillary fibres)
- CNIV, V (corneal sensation), VII, VIII palsies
- Hemiplegia (Weber)
- Tremor (Benedikt)
- Ataxia (Nothnagel)
- Tremor + Ataxia (Claude)
Aberrant regeneration of the third cranial nerve, or oculomotor synkinesis, refers to the abnormal response to firing of the oculomotor nerve causing paradoxical co-contraction of muscles. It is typical a result of an aneurysm or tumour in the cavernous sinus but can be seen following trauma to the third cranial nerve. The third cranial nerve supplies the superior rectus, inferior rectus, medial rectus, inferior oblique, the parasympathetically innervated pupil sphincter and levator palpebrae muscles. In aberrant regeneration after injury to the oculomotor nerve, fibres grow to supply other muscles, leading to co-contraction of these muscles (extraocular muscles, lid or pupil) on firing of the nerve.
Move the eye from full abduction (where there is no CNIII activation) to midline and then into adduction to see the full extent of the lid or pupil changes:
- Eyelid retraction / pupil constriction on adduction, upgaze and downgaze
- Paradoxical eye movements (i.e. adduction on attempted up / downgaze)
This can occur in the absence of other CNIII signs!
Aberrant regeneration doesn’t occur with “medical” causes (because the nerve sheath hasn’t been breached).
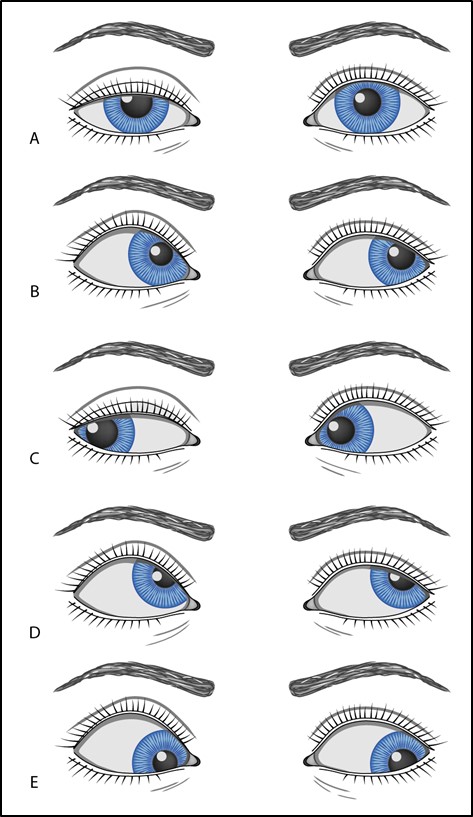
Figure 7.1.2
Right Cranial Nerve III Palsy with Aberrant Regeneration
A. Patient looking in primary position. Note the mild right upper lid ptosis and slightly dilated right pupil, consistent with a compressive cause.
B. Patient looking to the left (adduction). Note that the right pupil constricts (due to co-contraction of the parasympathetic fibres going to the pupillary sphincter). The right upper lid demonstrates prominent elevation (from co-contraction of the levator palpebrae). The adducting saccadic velocity of the right eye is reduced from incomplete recovery of the medial rectus function.
C. Patient is looking to the right (abduction). Note that right pupil is again slightly dilated and the right upper lid demonstrates mild ptosis, the same as they were in primary position (since there is no longer any firing of the oculomotor nerve).
D. Patient is looking up. The right pupil constricts and the upper lid elevates more than the left upper lid.
E. Patient is looking down. The right pupil constricts and the upper lid elevates more than the left upper lid.
Look for a concomitant CNIV palsy:
Look for intorsion (by observing the movement of the vessels on the conjunctiva) during attempted depression in abduction
OR
Check fundus to see if fovea is still (normally) below the optic disc (SO / CNIV and SR / CNIII intort the eye. Loss of intorters will cause fovea to be above the optic disc).
NB: This is only helpful in a complete CNIII palsy. If it is a partial CNIII palsy with SR still functional, this does not apply as the SR will still intort and hence the fovea will not necessarily be above the optic disc.
1. Complete CNIII Palsy
- Complete ptosis
- Pupil normal or enlarged
- Complete external ophthalmoplegia – no elevation, depression or adduction. Intact intorsion on attempted downgaze in abduction (CN IV) and abduction (CN VI)
2. Partial CNIII Palsy
- Can present with any deviation except ET
- Pupil enlarged
Summary
- Right or left
- Pupil involving or sparing
- Complete or incomplete
- Isolated or other associated CN palsies
- ± Aberrant regeneration?
Don’t miss: GCA, Aneurysm, Pituitary apoplexy, cavernous sinus thrombosis.
1. Idiopathic
2. Pupil Sparing (“Medical” Causes)
Microvascular
HT, Cholesterol, DM, smoking
Inflammatory
GCA, Vasculitis, Sarcoidosis
Infective
HZO, Syphilis
3. Pupil Involving (“Surgical” > “Medical” Causes)
Vascular
Posterior communicating artery aneurysm (assume this unless proven otherwise), ICA aneurysm, Subarachnoid haemorrhage, carotico-cavernous fistula, cavernous sinus thrombosis, pituitary apoplexy
Neoplastic
Glioma, meningioma, nasopharyngeal carcinoma
Inflammatory
IOID (Tolosa-Hunt syndrome)
Infective
Meningitis / encephalitis / abscess
Trauma / Surgical
Subarachnoid, extradural haemorrhage → uncal herniation
NB: Pain does not distinguish between ischaemic microvascular disease and a compressive lesion.
- CT(A) / MRI(A) [i] brain – must be with contrast agent
- Pupil involving
- Pupil sparing partial
- Pupil sparing complete AND:
- <50 years
- Other CN palsies
- Progressive
- Aberrant regeneration
- BP, BSL / HbA1C, Lipids (for Vascular risk factors)
- ± ESR / CRP (for GCA)
- ± Vasculitic screen, ACE, Syphilis serology
- ± Tests for Myasthenia (not necessary if there is pupil involvement since this does not occur in MG)
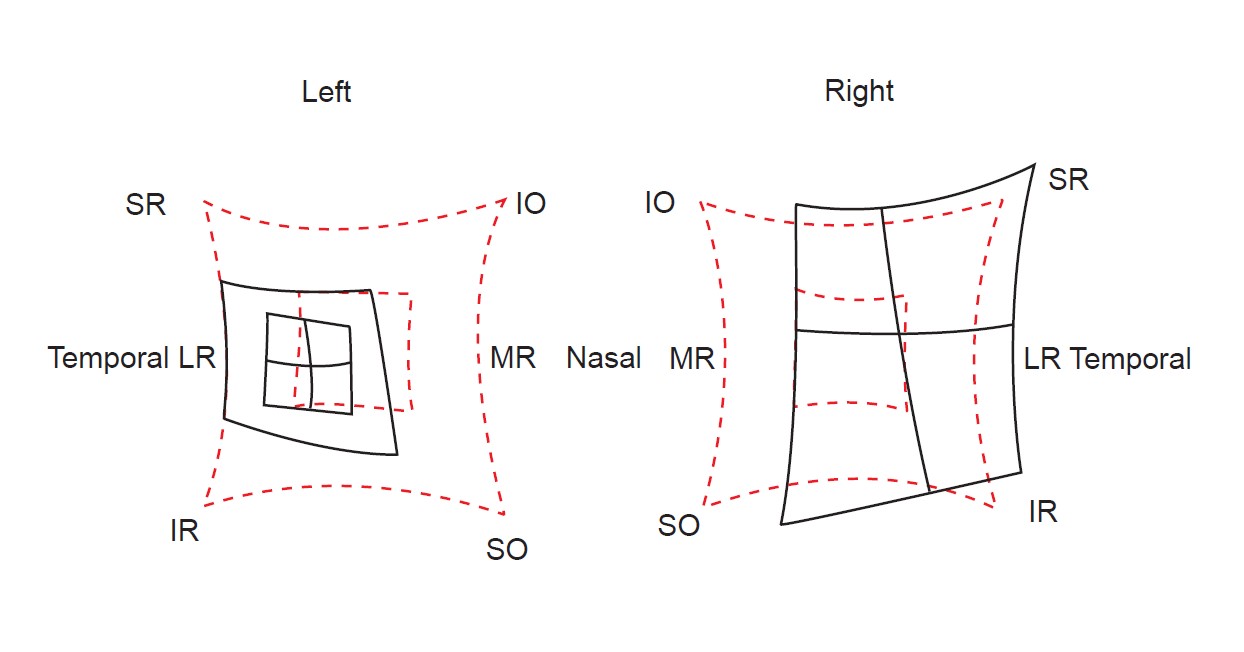
- Hess (left CNIII palsy)
- Contraction of L, expansion of R
- L exotropia
- L chart: Underaction of all muscles except the LR and SO
- R chart: Overaction of all muscles except the MR and IR (yokes of the spared muscles)
MRA has extremely high sensitivity for all causes of CNIII, no radiation and gives the added benefit of looking for demyelination BUT must requires a 3 Tesla magnet (difficult to get urgently) and patients may become claustrophobic. CTA is much more sensitive for detection of posterior communicating aneurysms, gives more “anatomic” detail than MRA (for neurosurgeons), is easier to obtain and is quicker. Digital angiography can be used if CTA / MRA is not possible.
See Li Q, Lv F, Li Y, Luo T, Li K, Xie P. Evaluation of 64-section CT angiography for detection and treatment planning of intracranial aneurysms by using DSA and surgical findings. Radiology. 2009;252(3):808‐815. doi:10.1148 / radiol.2523081911 for more information.
Treat the underlying cause (e.g. aneurysm, diabetes, hypertension).
Indications for treatment:
- Abnormal head posture
- Diplopia
- Cosmesis
Aims:
- Correct AHP
- Maximise field of BSV
- Align eyes in primary for cosmesis
- Uniocular occlusion for diplopia of the non-dominant eye once ptosis lifts
- Fresnel prism
- Not very effective since the squint is incomitant and often large
- Botulinum toxin into ipsilateral LR
- Cosmetic improvement
- But only temporary, doesn’t improve BSV
- Wait at least 12 months (deviation must be stable)
- Difficult surgery, minimize patient expectations especially if complete
If Partial Paralysis…
- Recess (LR) / Resect (MR) (may supra-place muscles for hypotropia)
- ± Recess LR of contralateral eye if deviation is very large
If Complete Paralysis
(no duction, poor saccade, poor forced generation test)
- Maximally recess (LR) / Resect (MR)
- OR attach lateral rectus to the periosteum
- NB: Beware of lifting the eyelid as this may unmask diplopia / cause exposure!
1. CNIII Nucleus
- Typical ocular motility defects (but bilateral superior rectus dysfunction 4) +
- Bilateral ptosis (single central caudal nucleus innervates both levators) +
- Pupil involving (Edinger-Westphal nucleus lies cranially)
2. Fasciculus (Outside Nucleus but Within Midbrain)
E.g. Occlusion of perforating branches of PCA.
- Typical ocular motility defects +
Weber Syndrome
Contralateral hemiplegia (corticospinal tract in cerebral peduncle)
Benedikt Syndrome
Tremor (red nucleus)
Nothnagel’s Syndrome
Contralateral ataxia (superior cerebellar peduncle)
Claude’s Syndrome
Tremor (red nucleus) + Contralateral ataxia (superior cerebellar peduncle)
Previous
7.0 Introduction
All rights reserved. No part of this publication which includes all images and diagrams may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the authors, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law.
Vitreoretinal Surgery Online
This open-source textbook provides step-by-step instructions for the full spectrum of vitreoretinal surgical procedures. An international collaboration from over 90 authors worldwide, this text is rich in high quality videos and illustrations.