1.2 Anterior Segment Differential Diagnoses and Aetiologies
When describing differential diagnoses, try to categorise your list into either:
- Most common first
- Most serious first
- Pathological sub-groups (e.g. infection, neoplasia etc.)
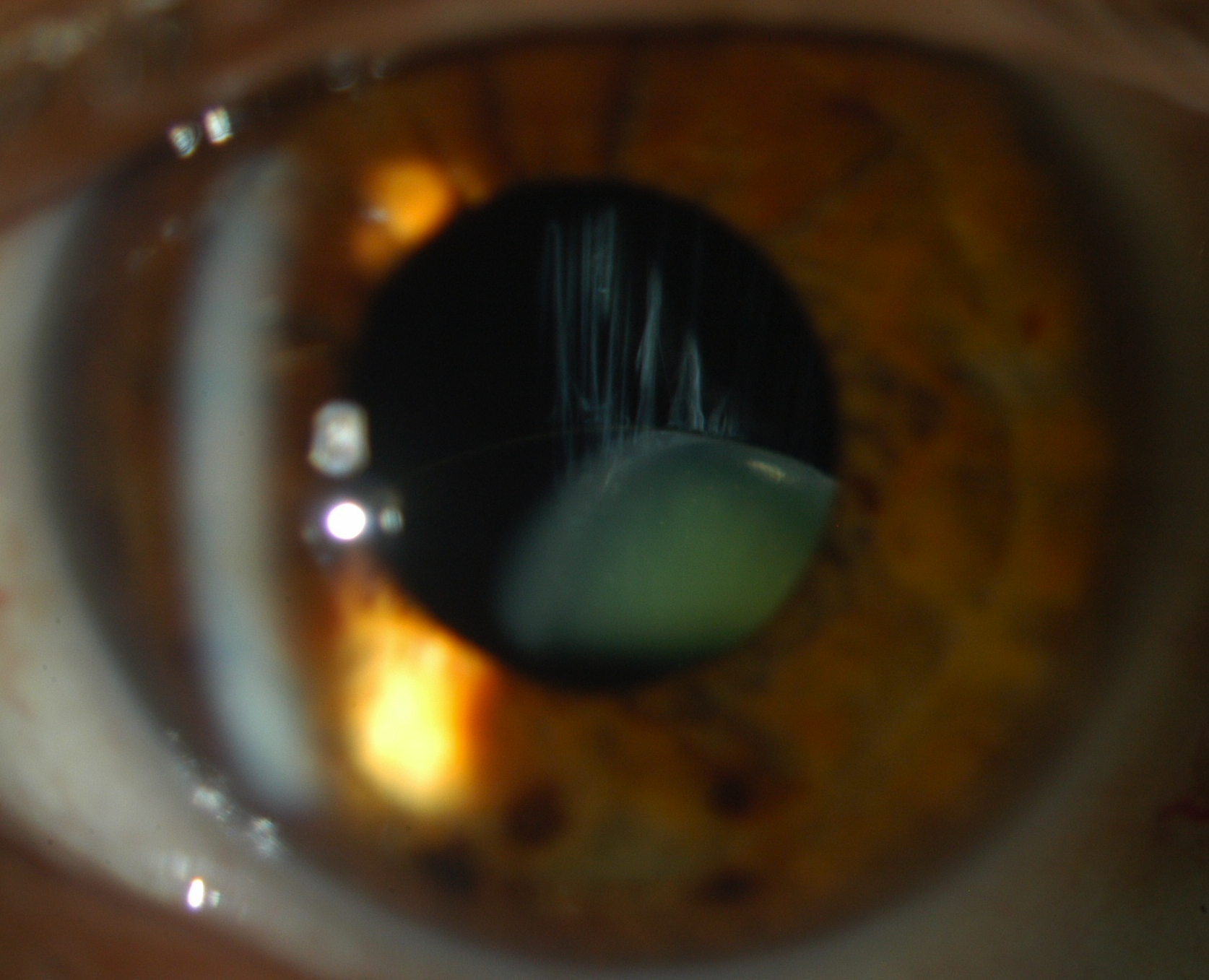
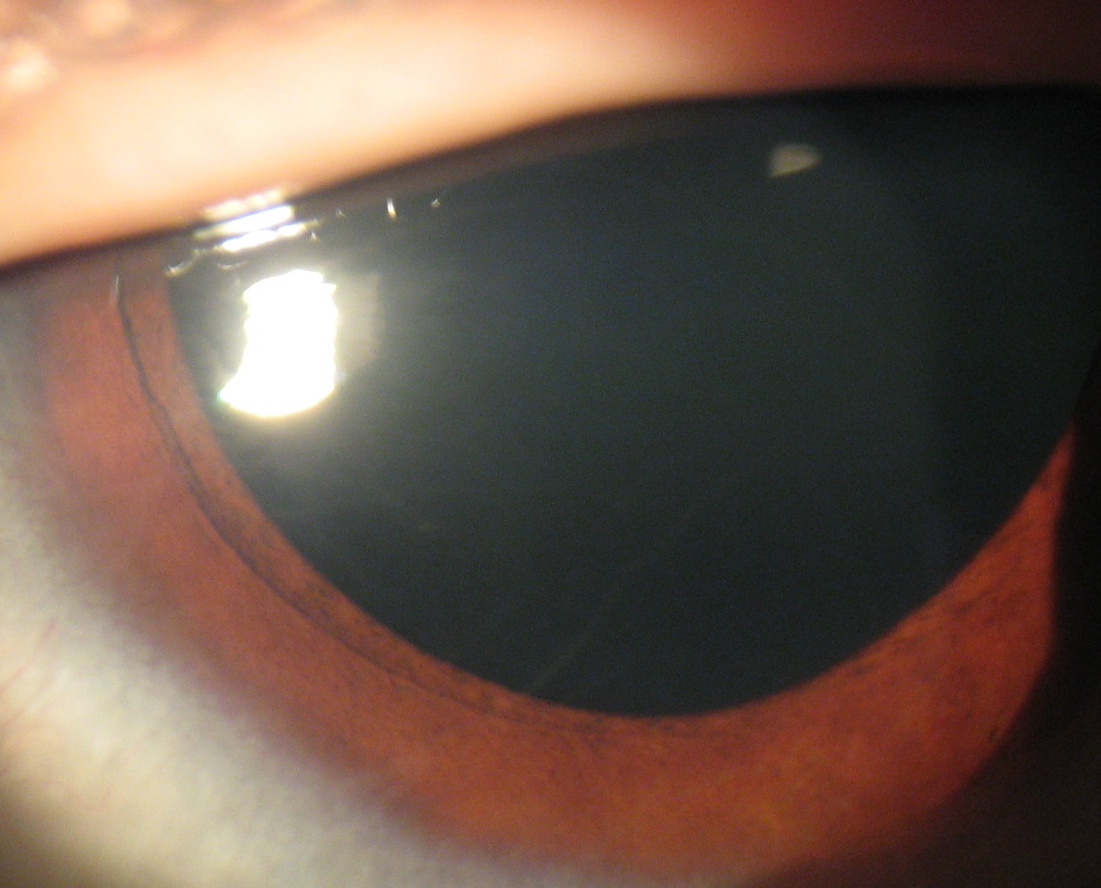
- Cataract (Congenital)
- Cataract (Unilateral)
- Conjunctival Follicles “LID”
- Conjunctival (Non-Pigmented) Tumours
- Conjunctival (Pigmented) Lesions
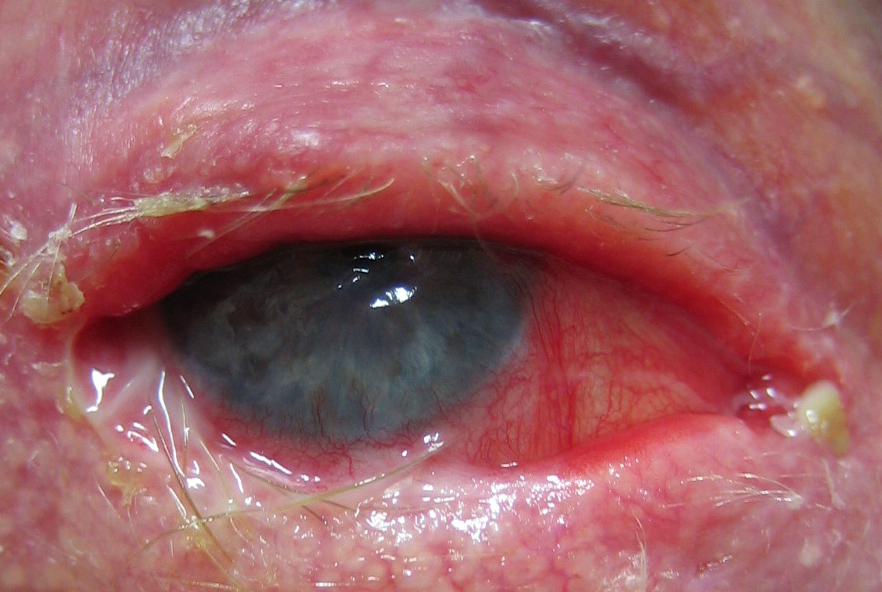
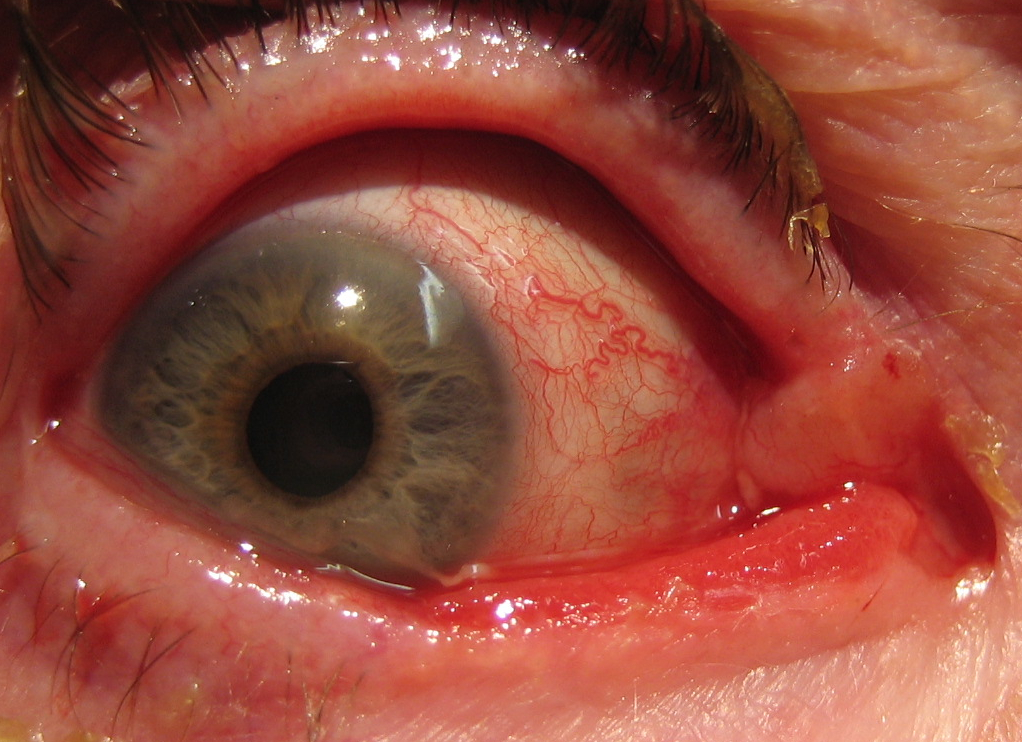
- Conjunctivitis – Cicatrising
- Contact Lens Associated Red Eye (CLARE)
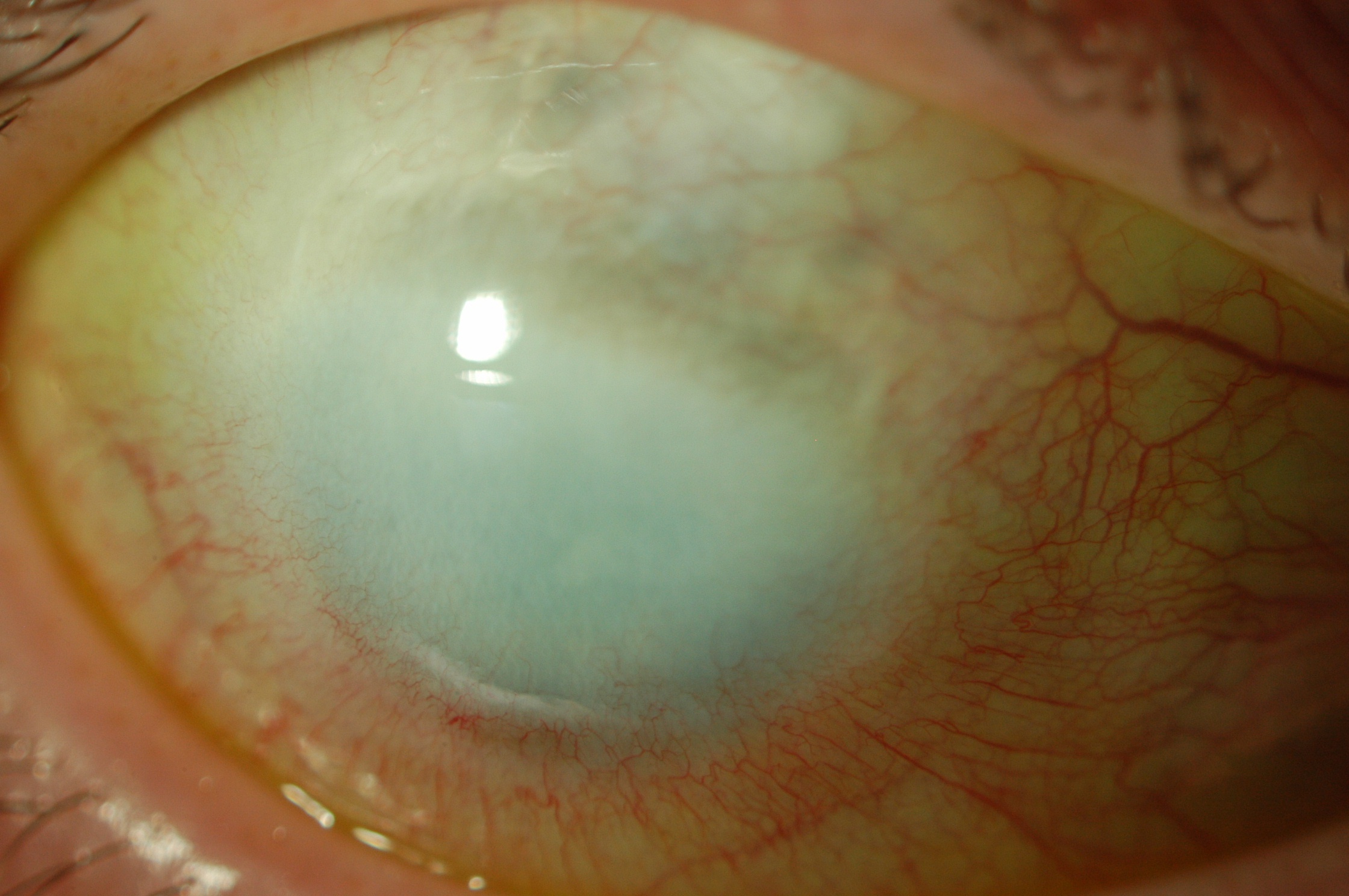
- Cornea – Congenital Opacities
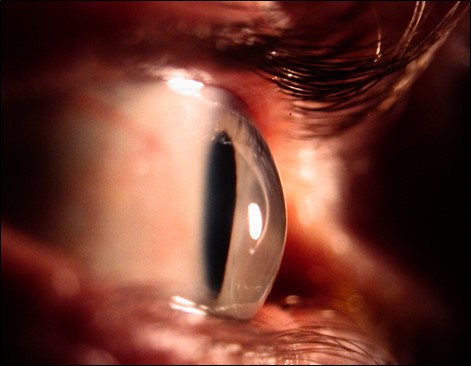
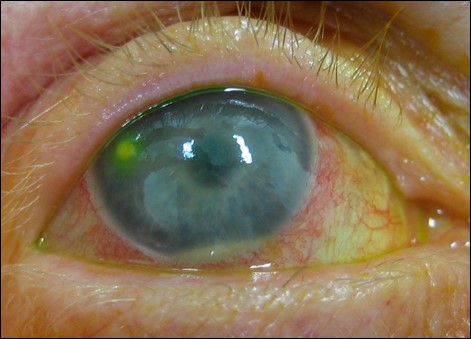
- Corneal Ectasia
- Corneal Thinning – Peripheral
- Ectopia Lentis
- Ectropion Uveae
- Enlarged Corneal Nerves
- Eyelash (Madarosis)
- Eyelash (Poliosis)
- Eyelash (Trichomegaly)
- Eyelid Lesions (Benign)
- Eyelid Lesions (Malignant)
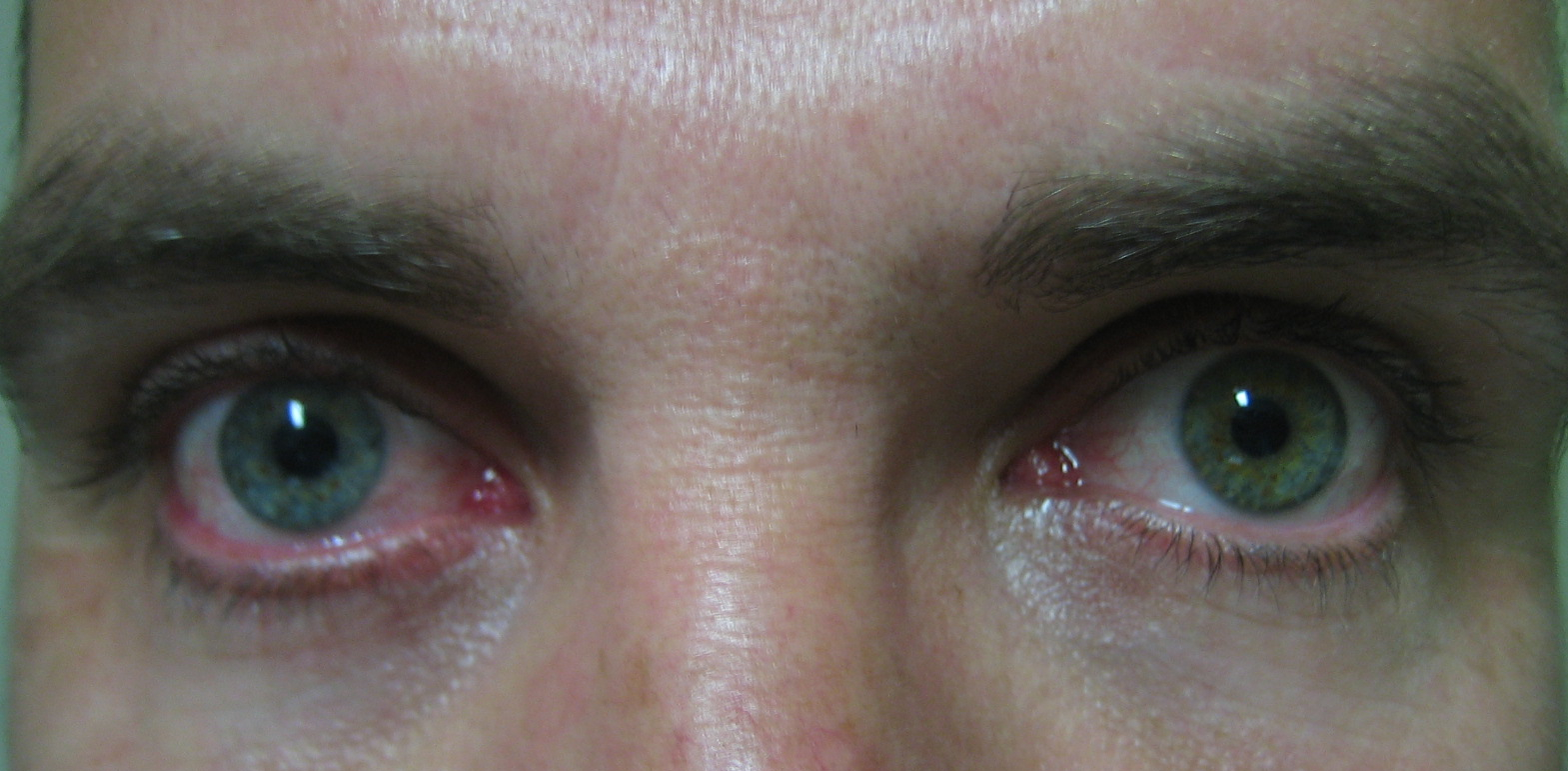
- Heterochromia Iridis
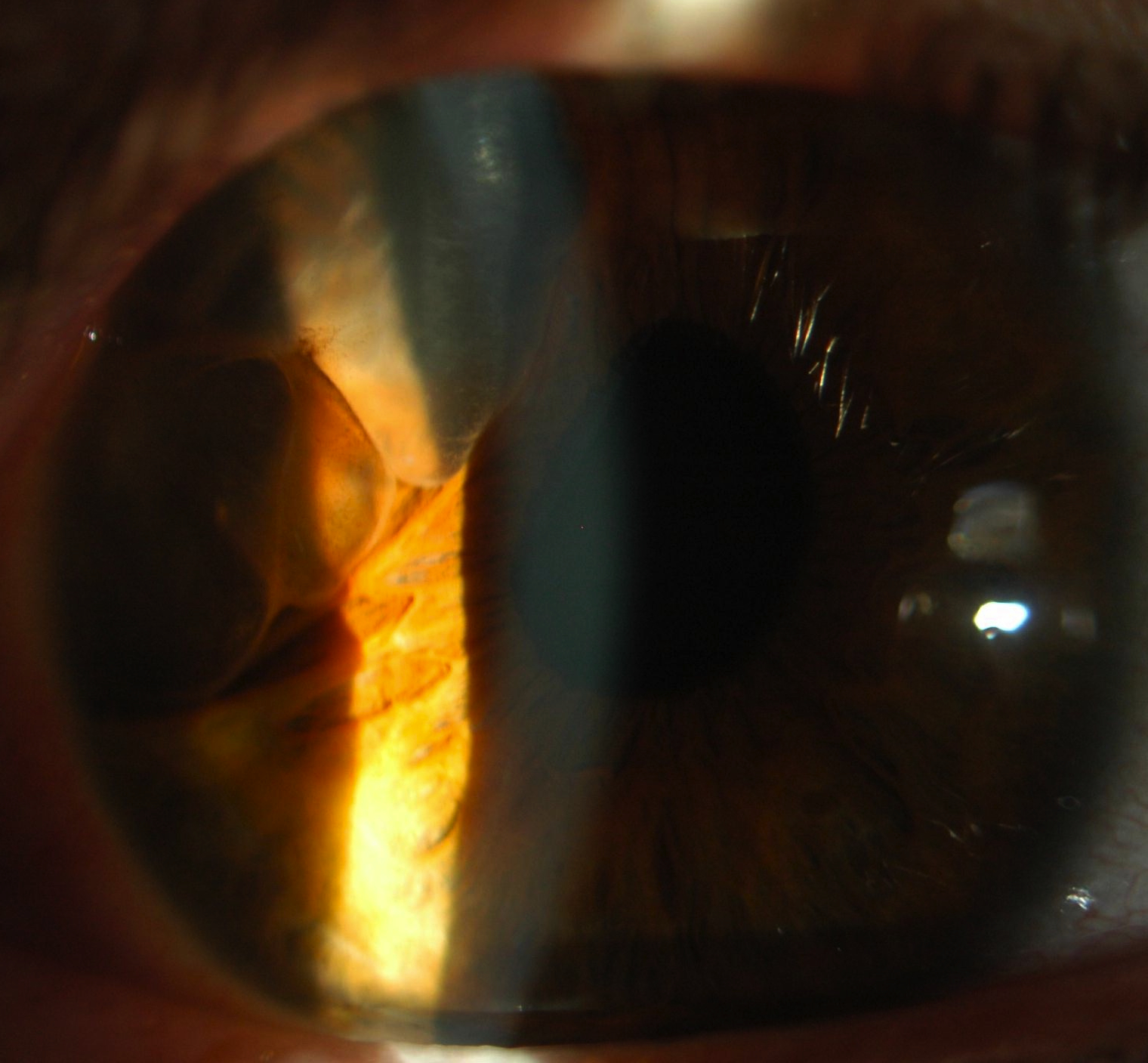
- Hyphaema
- Iris Lesions
- Iron Deposition Lines
- Keratitis
- Keratitis – Filamentary
- Keratitis – Interstitial
- Leucocoria
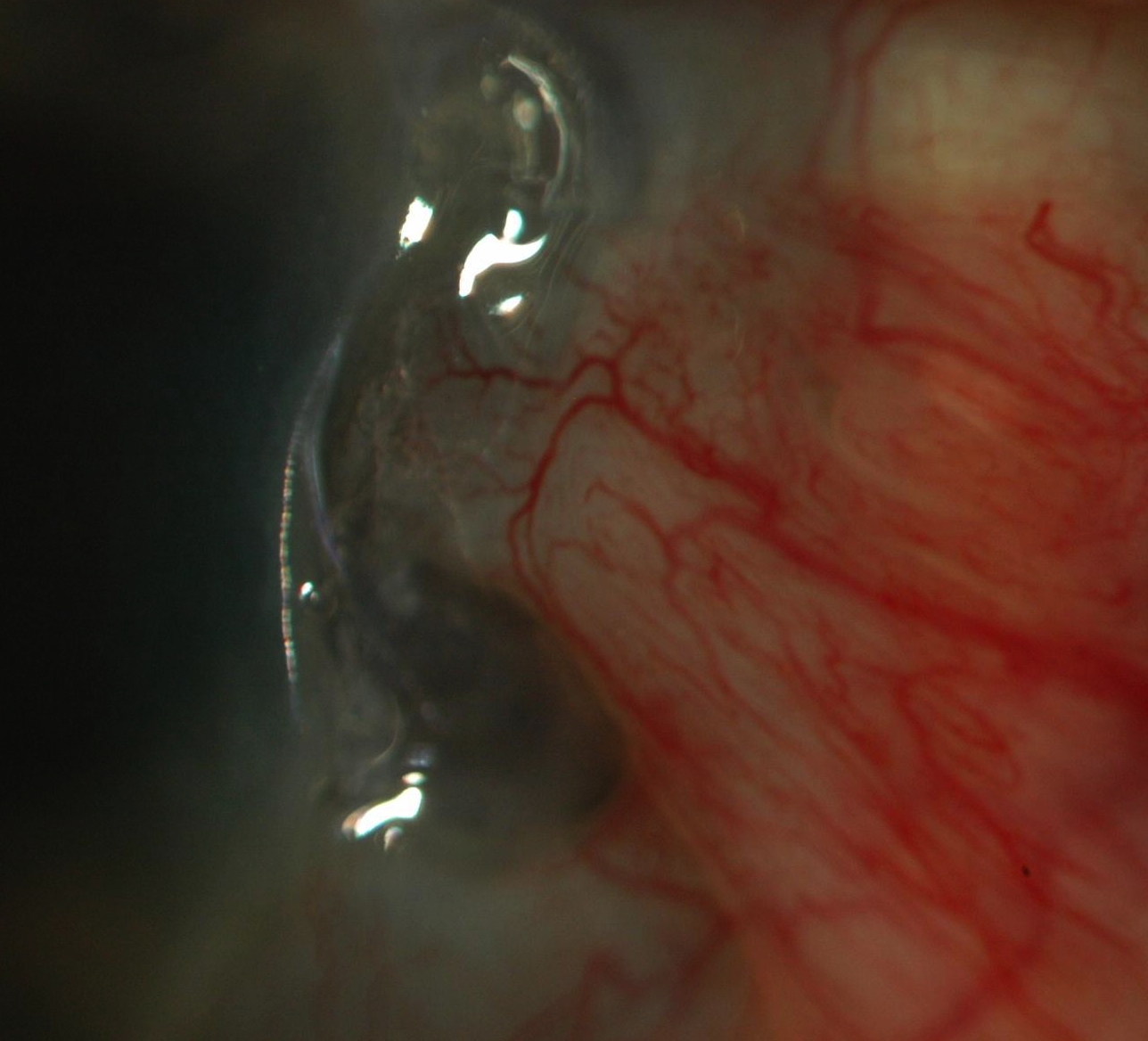
- Limbal Stem Cell Failure
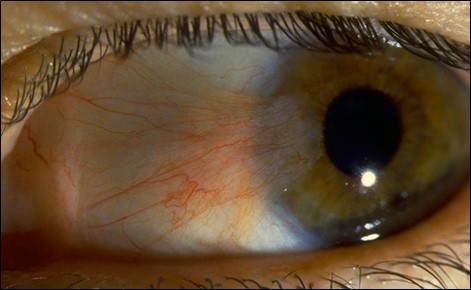
- Pterygium
- Recurrent Epithelial Erosions
- Sclera – Blue
- Vortex Keratopathy (Cornea Verticillata)
Always stand back and examine the patient as a whole. Age / gender / ethnicity are often useful in narrowing the potential differential diagnoses. Iris heterochromia, symblephara, ankyloblepharon and forniceal shortening are often more obvious on gross inspection before beginning the slit lamp examination.
A. Isolated
- Sporadic (1/3): Unilateral (“two-hit” hypothesis)
- Hereditary (1/3): Bilateral 75% AD
B. Associated Syndrome, Ocular or Systemic Disease (1/3, Bilateral) “MAGIC”
Metabolic
- Hypoglycaemia
- Galactosaemia (oil drop cataract)
- Wilson Disease
- Alport Syndrome
- Lower Syndrome
Anterior Segment Dysgenesis
- Axenfield-Reiger
- Peters
- Aniridia
Genetic
- Autosomal Dominant
- Marfan Syndrome
- Myotonic Dystrophy
Infections
- TORCH/Syphilis
Chromosomal
- Down Syndrome
- Patau Syndrome
- Edward Syndrome
C. Trauma
D. Steroids
- JIA in young children
E. Radiation
- Trauma
- Post-Vitrectomy
- Steroid Drops
- Uveitis (e.g. Fuchs heterochromic iridocyclitis)
- Atopy
- Malignancy
- Lymphoma
- Infectious
i. Viral: Adenoviral, Molluscum, Herpetic
ii. Bacterial: Chlamydia, Gonorrhea - Drugs
i. Briminodine
Not allergic!
NB: Papillae are non-specific
- Papilloma
- Conjunctival intraepithelial neoplasia (CIN)
- SCC
- Amelanotic melanoma
- Lymphoma
- Pterygium
- Conjunctival epithelial (racial) melanosis
- Congenita locular melanocytosis
- Conjunctival Naevus
- Primary Acquired Melanosis
- Melanoma
Burns
Chemical (alkali), Radiation
OCP
SJS/TEN
Inflammatory
Rosacea, Graft vs Host disease, Atopic Conjunctivitis
Iatrogenic
Drops (Pilocarpine)
Infections
Trachoma
"S"
Sjogrens (dry eye), Scleroderma, Sarcoidosis
- Infective: Microbial keratitis
- Non-infective: If in doubt, treat as infective
i. Hypoxia
ii. Trauma
iii. Sterile infiltrate (immune response)
iv. Toxicity / allergy to solutions
v. Giant papillary conjunctivitis
“STUMPED”
- S clerocornea
- T ears in DM = Haab striae (congenital glaucoma); Trauma (birth)
- U lcer (HSV, Bacterial, Neurotrophic)
- M etabolic (Mucopolysaccharidoses, Mucolipidosis, Tyrosinemia)
- P eters, Posterior keratoconus
- E ndothelial (CHED, CHSD)
- D ermoid
- Keratoconus
- Pellucid marginal degeneration
- Keratoglobus
- Post-LASIK
Local
Systemic
Non-Infective
Local
- Trauma
- Marginal keratitis
- Terrien (perforation is rare)
- Mooren (diagnosis of exclusion)
- Pellucid marginal degeneration
- Dellen
- Drugs (steroids, NSAID, LA)
Systemic
- Sjogren (Dry Eye)
- RA
- SLE
- Rosacea
- PAN
- Wegener Granulamotosis
Infective
Local
- HSV, HZO (neurotrophic cornea)
- Gonorrhoea, Chlamydia
Systemic
- TB
- Syphilis
- HCV
Inherited Without Systemic Associations
- Familial ectopia lentis (AD)
- Aniridia (AD)
- Ectopia lentis et pupillae (AR)
Inherited With Systemic Associations
- Marfan syndrome (AD)
- Homocystinuria (AR)
- Ehlers-Danlos 6 (AR)
- Weill-Marchesani syndrome (AD/AR)
- Stickler syndrome (AD)
- Sulphite oxidase deficiency (AR)
- Hyperlysinaemia (AR)
Non-Inherited
- Trauma
- Pseudoexfoliation
- Large eye (High myope, buphthalmos)
- Anterior uveal tumour
- Hypermature cataract
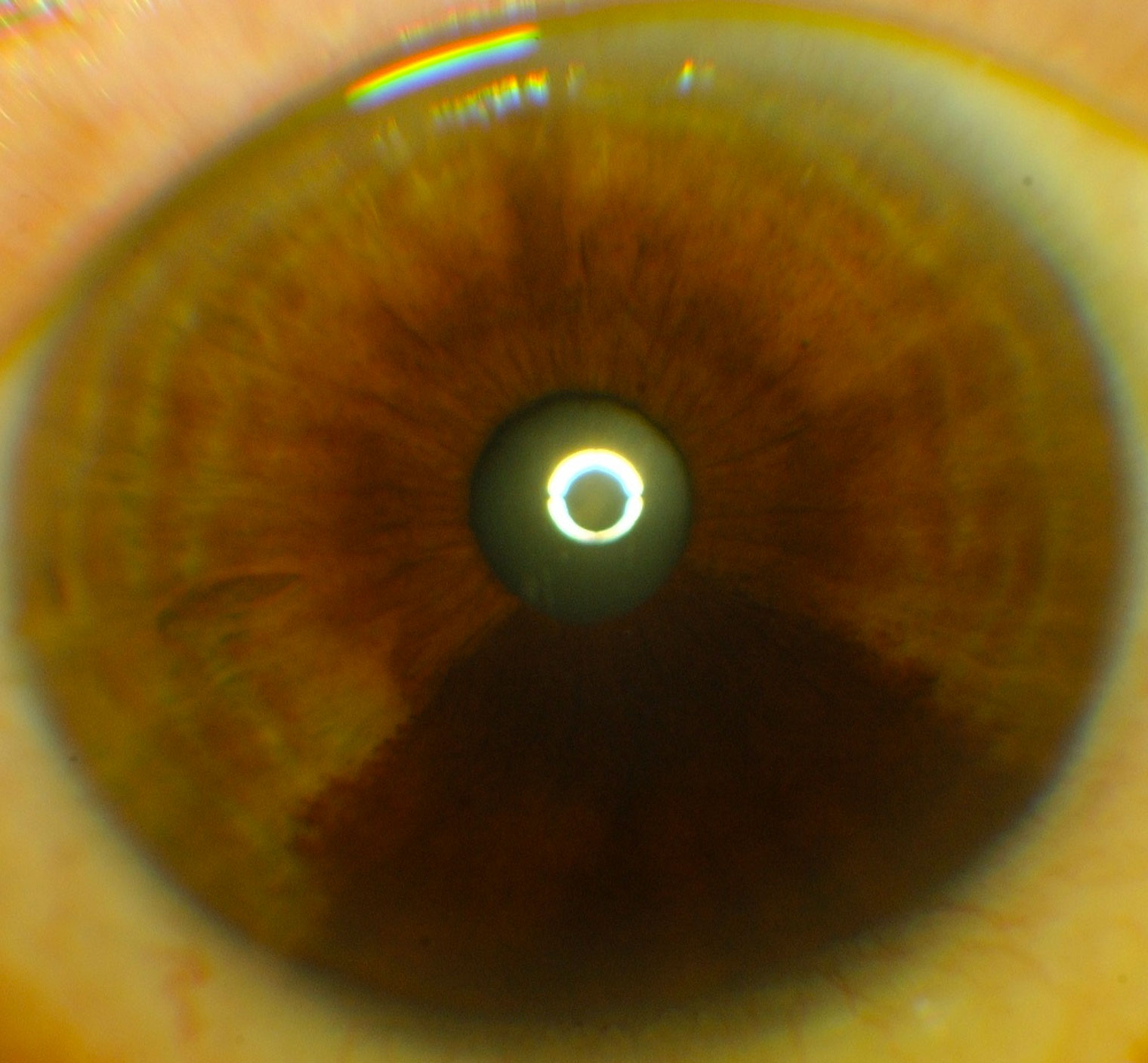
Congenital
- ICE
- NF-1
Acquired
- NVI
- Iris tumours
- Uveitis
- Epithelial ingrowth
“KAFMINA”
- K eratoconus
- A canthamoeba keratitis
- F uchs endothelial dystrophy
- M EN IIb
- I chthyosis, Idiopathic
- N F-1
- A myloidosis
Local
- Blepharitis
- Tumours (BCC, SCC, melanoma)
- Burns
- Radiotherapy
- Cryotherapy
Dermatological
- Alopecia
- Psoriasis
Systemic
- Hypothyroidism
- SLE
- Syphilis
- Leprosy
Removal
- Iatrogenic
- Trichotillomania
- Blepharitis
- VKH, Sympathetic ophthalmia
- Vitiligo
- Tuberous sclerosis
- Marfan syndrome
- Drugs (Latanoprost, phenytoin, cyclosporin)
- Malnutrition
- HIV
- Hypothyroidism
- Oculocutaneous albinism
- Squamous cell papilloma
- Basal cell papilloma, Seborrheic keratosis
- Actinic keratosis
- Melanocytic naevus
- Keratoacanthoma
- Chalazion/hordeolum
- BCC
- SCC
- Sebaceous gland carcinoma
- Melanoma
- Kaposi sarcoma
- Merkel cell carcinoma
- Lymphoma
- Metastasis
Hypochromia
- Fuchs uveitis (lighter)
- Horner’s (congenital)
- Uveitis (e.g. HZO atrophy)
- JXG
Hyperchromia
- Latanoprost
- Oculodermal melanocytosis (naevus of Ota), Naevus (diffuse, including ICE), Melanoma
- PDS
- Ocular siderosis
- Sturge-Weber syndrome (rare)
Hypochromia
- Fuchs uveitis (lighter)
- Horner’s (congenital)
- Uveitis (e.g. HZO atrophy)
- JXG
Hyperchromia
- Latanoprost
- Oculodermal melanocytosis (naevus of Ota), Naevus (diffuse, including ICE), Melanoma
- PDS
- Ocular siderosis
- Sturge-Weber syndrome (rare)
- Melanoma
- Naevus
- Cyst
- Metastasis (lung or breast): Often bilateral / multiple, amelanotic, variable size / colour
- Adenoma / Adenocarcinoma of the iris posterior pigment epithelium
- Leiomyoma
- Lisch nodules
- Juvenile xanthogranuloma
- Brushfield spots (Down syndrome)
- Foreign body
- Hudson-Stahli (elderly)
- Fleischer (Keratoconus)
- Stocker (Pterygium)
- Ferry (Trabeculectomy)
- Bacterial
- Viral (herpetic)
- Fungal
- Protozoa (Acanthamoeba)
- Mycobacterial
- Dry eye
- Superior limbic keratitis
- Recurrent erosion syndrome
- Neurotrophic keratitis
- Contact lens, patching
Infectious
- Congenital syphilis
- HSV, VZV, EBV
- Chlamydia
- TB
- Leprosy
- Acanthamoeba
Non-infectious
- Cogan syndrome
- Sarcoidosis
- Behcet’s
- Gold
“CARPET”
- C oats, Cataract
- A strocytoma
- R etinoblastoma, ROP
- P HPV
- E ndophthalmitis
- T oxocara
+ Incontinentia pigmenti
+ Intermediate uveitis
A. Genetic
- Aniridia
- Peters anomaly
- Xeroderma pigmentosa
B. Acquired
“TAINT”
Traumatic
- Chemotherapy
- Radiation
- Contact lens overuse
- Limbal surgery
Autoimmune
- SJS
- OCP
- GvHD
- VKC
Infective
- Bacteria – trachoma
- Viral -HSV
- Fungal
Neoplastic
- Ocular surface tumours
- Pterygium/Pseudopterygium
Toxic
- Preservatives
- Pingueculum
- Pseudopterygium
- OSSN/CIN
- Pannus
- Corneal trauma
i. Minor trauma (especially organic), LASIK - Corneal dystrophy
i. Epithelial BM dystrophies – Reis buckler, Thiel Bentke, Meesmann
ii. Stromal dystrophies - Corneal degeneration
i. Band, Salzmann - Neurotrophic cornea
- Bullous keratopathy
- Ocular surface problems
- Lagophthalmos
- P seudoxanthoma elasticum
- O steogenesis imperfecta
- E hlers Danlos
- M arfan syndrome
“FLATCAN”
- F abry disease
- X-linked recessive Lipid storage disorder (Lysosomal α-galactosidase-A deficiency)
- Vortex keratopathy, cataract, conjunctival & retinal vessel tortuosity, cutaneous angiokeratomas, CVS, renal disease
- L imbal stem cell failure
- A miodarone
- T amoxifen
- C hloroquine/ Hydroxychloroquine
- A tovaquone
- N SAIDS
All rights reserved. No part of this publication which includes all images and diagrams may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the authors, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law.
Vitreoretinal Surgery Online
This open-source textbook provides step-by-step instructions for the full spectrum of vitreoretinal surgical procedures. An international collaboration from over 90 authors worldwide, this text is rich in high quality videos and illustrations.