9 Investigations
9.1 Corneal Topography and Tomography
9.2 Confocal Microscopy
9.3 Optical Coherence Tomography - Macula
9.4 Optical Coherence Tomography Angiography (OCT-A)
9.5 Optical Coherence Tomography - Glaucoma
9.6 Optical Coherence Tomography – Anterior Segment
9.7 Fundus Autofluorescence Imaging
9.8 Fundus Angiography - Fluorescein
9.9 Fundus Angiography - Indocyanine Green
9.10 B-scan Ultrasonography & UBM
9.11 Electrophysiology
9.12 Automated Visual Fields
9.13 Neuroimaging
9.8 Fundus Angiography - Fluorescein
Fundus fluorescein angiography (FFA) provides valuable information regarding fundus pathology. Intravenous fluorescein is injected, which remains in the retinal vasculature and is freely permeable to the choriocapillaris. It is impermeable to an intact blood-retinal barrier (retinal vessel walls and the retinal pigment epithelium (RPE)). Fluorescein absorbs blue light (wavelength 490nm) and emits yellow-green light (wavelength 530nm). A yellow-green barrier filter removes un-fluoresced reflected light wavelengths. A fundus camera is therefore able to detect the location of the fluorescein dye. Colour and red free photographs are usually taken prior to commencing FFA. All FFA’s should be read in conjunction with the clinical history and examination. It is important to recognise that this is a dynamic test.
The phases of FFA are as follows:
1. Choroidal Filling (10 - 15s)
- This provides a background flush that may be patchy in appearance. The time for choroidal filling can be highly variable, depending on the nature of the vein and cannula that the intravenous fluorescein is injected
2. Arterial Filling (1 - 3s Later)
3. Arteriovenous Phase
- Laminar flow is observed along venous walls
4. Venous Phase
- The arterio-venous (AV) transit time is calculated from the time it takes for fluorescein to first appear in the temporal retinal arteries, to the time that the corresponding temporal retinal veins are completely filled. This is usually under 12s
5. Late Phase
- Fluorescein recirculates back into the retinal arterial system after ~60s. By ~10 minutes fluorescein is no longer evident
1. Leakage
- Vessels that leak demonstrate hyperfluorescence that increases with time. This occurs with breakdown of the blood-retinal barrier such as in: retinal neovascularisation (pre-retinal), “choroidal” neovascularisation (sub-RPE/Type1, sub-retinal/Type 2, intra-retinal/Type 3) and macular oedema
2. Staining
- Some structures (drusen, fibrosis) absorb fluorescein and slowly increase in hyperfluorescence. These structures retain some fluorescence even after it has been eliminated from the retinal and choroidal circulations
3. Window Defect
- Window (transmission) defects typically occur when there is absence of the RPE, as occurs with geographic atrophy in atrophic age-related macular degeneration or following retinal laser scars. Background choroidal hyperfluorescence is clearly seen without the interference of RPE melanin and lipofuscin. Fluorescence increases then fades, without extending beyond the boundaries of the window defect
4. Pooling
- Pooling occurs when fluorescein accumulates in an empty space. Examples include central serous chorioretinopathy (hyperfluorescence increases in intensity and size until the borders of the serous retinal detachment are reached) and serous pigment epithelial detachments (hyperfluorescence increases in intensity but due to rapid early filling of the PED with fluorescein, it does not increase in size)
1. Avascular Zones
- The foveal avascular zone (usually 500µm) is hypofluorescent because it does not contain retinal capillaries. In addition, choroidal fluorescence is blocked by retinal xanthophyll and RPE melanin and lipofuscin. Lack of choroidal hyperfluorescence is also seen with capillary nonperfusion (such as in proliferative diabetic retinopathy or an ischaemic central retinal vein occlusion). Retinal artery occlusions are characterised by hypofluorescence in the vessel distal to the occlusion
2. Blocked Fluorescence
- Fluorescence can be blocked by structures that do not fluoresce. The degree of blocked fluorescence depends on the depth of blocking structure in relation to the retina. Pre-retinal haemorrhage will block all fluorescence; retinal and RPE lesions (deep haemorrhages, exudate, pigment) will block choroidal fluorescence
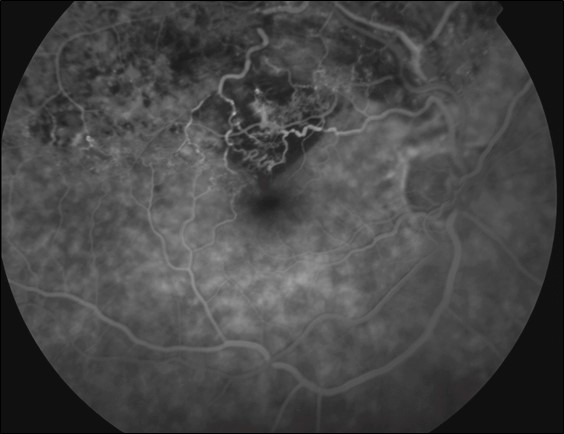
- Figure 9.8.2: Acute Posterior Multifocal Placoid Pigment Epitheliopathy (APMPPE)
- Figure 9.8.3: Adult Vitelliform Macular Degeneration
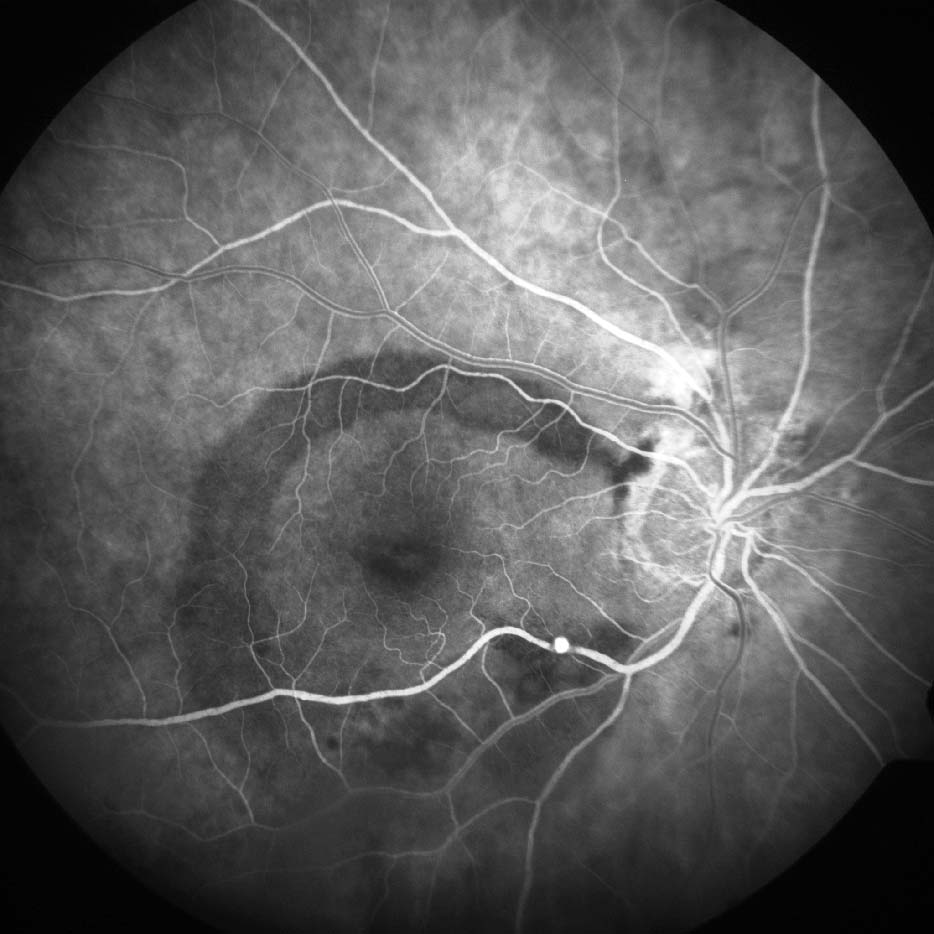
- Figure 9.8.4: Branch Retinal Vein Occlusion
- Figure 9.8.5: Branch Retinal Vein Occlusion
- Figure 9.8.6: Central Serous Chorioretinopathy
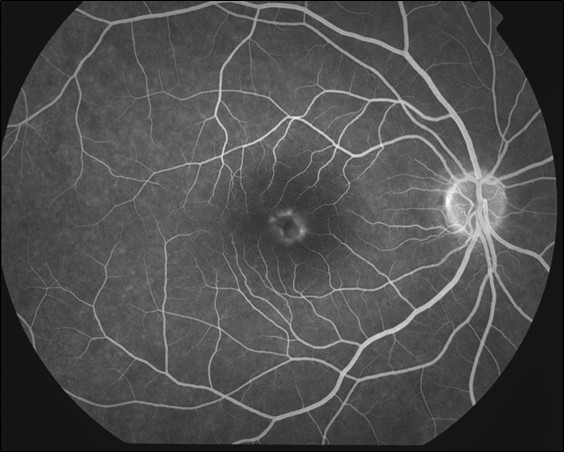
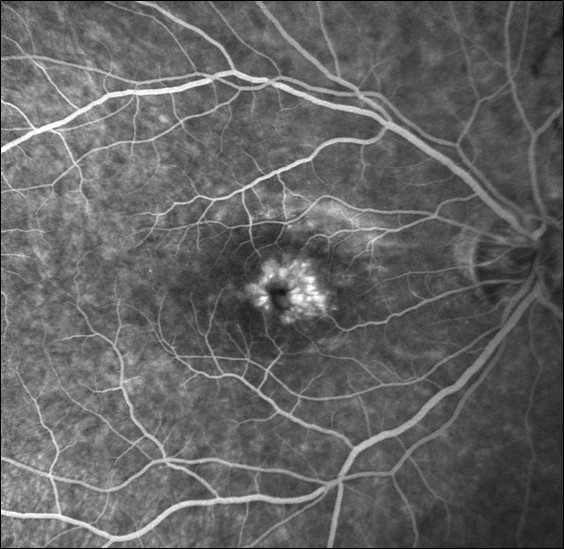
- Figure 9.8.7: (Classic Subfoveal) Choroidal New Vessel
- Figure 9.8.8: Coats Disease
- Figure 9.8.9: Cystoid Macular Oedema
- Figure 9.8.10: Fundus Flavimaculatus (ABCA4 gene mutation)
- Figure 9.8.11: Hemi-retinal artery occlusion
- Figure 9.8.12: Hypertensive Retinopathy
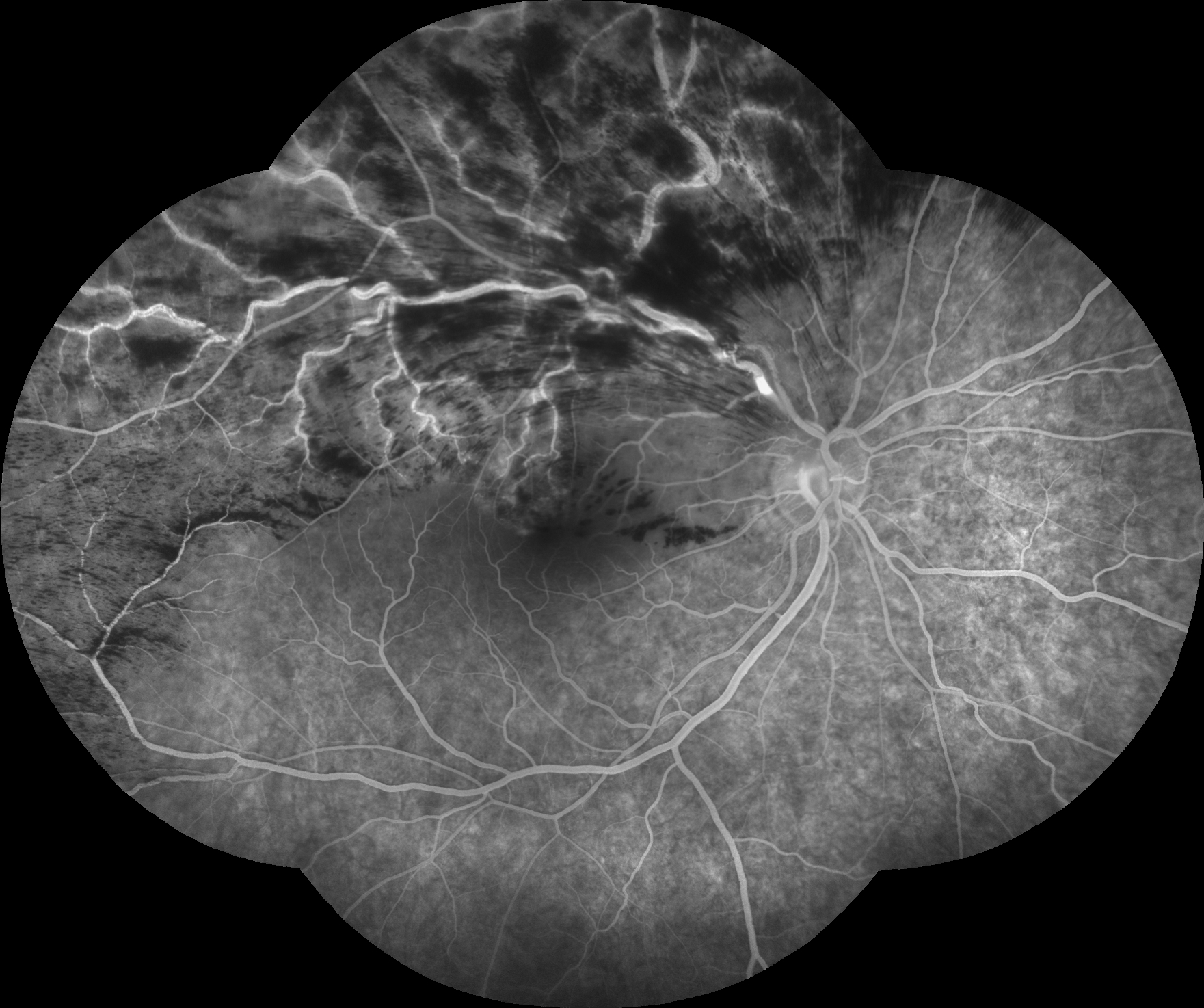
- Figure 9.8.13: Neovascularisation of the optic disc (NVD)
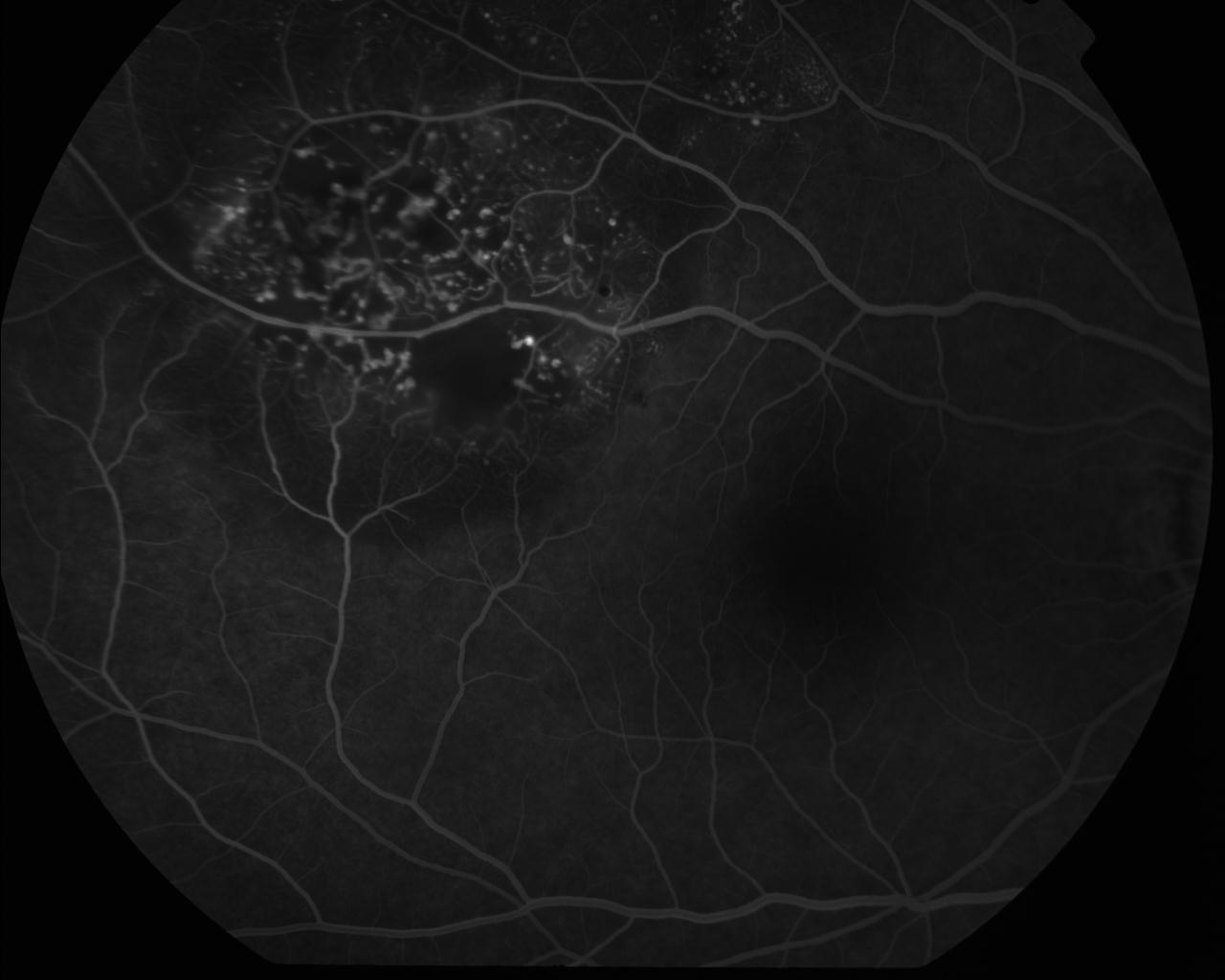
- Figure 9.8.14: Proliferative Diabetic Retinopathy
- Figure 9.8.15: Proliferative Diabetic Retinopathy (Optos®)
- Figure 9.8.16: Retinal Arteriolar Macroaneurysm
- Figure 9.8.17: Retinal Macroaneurysm
- Figure 9.8.18: Retinal Macroaneurysm (Ruptured)
- Figure 9.8.19: Retinopathy of Prematurity
- Figure 9.8.20: RPE Rip
- Figure 9.8.21: Sarcoid Periphlebitis
- Figure 9.8.22: Serous PED
- Figure 9.8.23: Sickle Cell Disease
- Figure 9.8.24: Stargardt Disease
- Figure 9.8.25: Susac Syndrome
- Figure 9.8.26: Vasoproliferative Tumour
- Figure 9.8.27: Vogt-Koyanagi-Harada disease
.jpg)
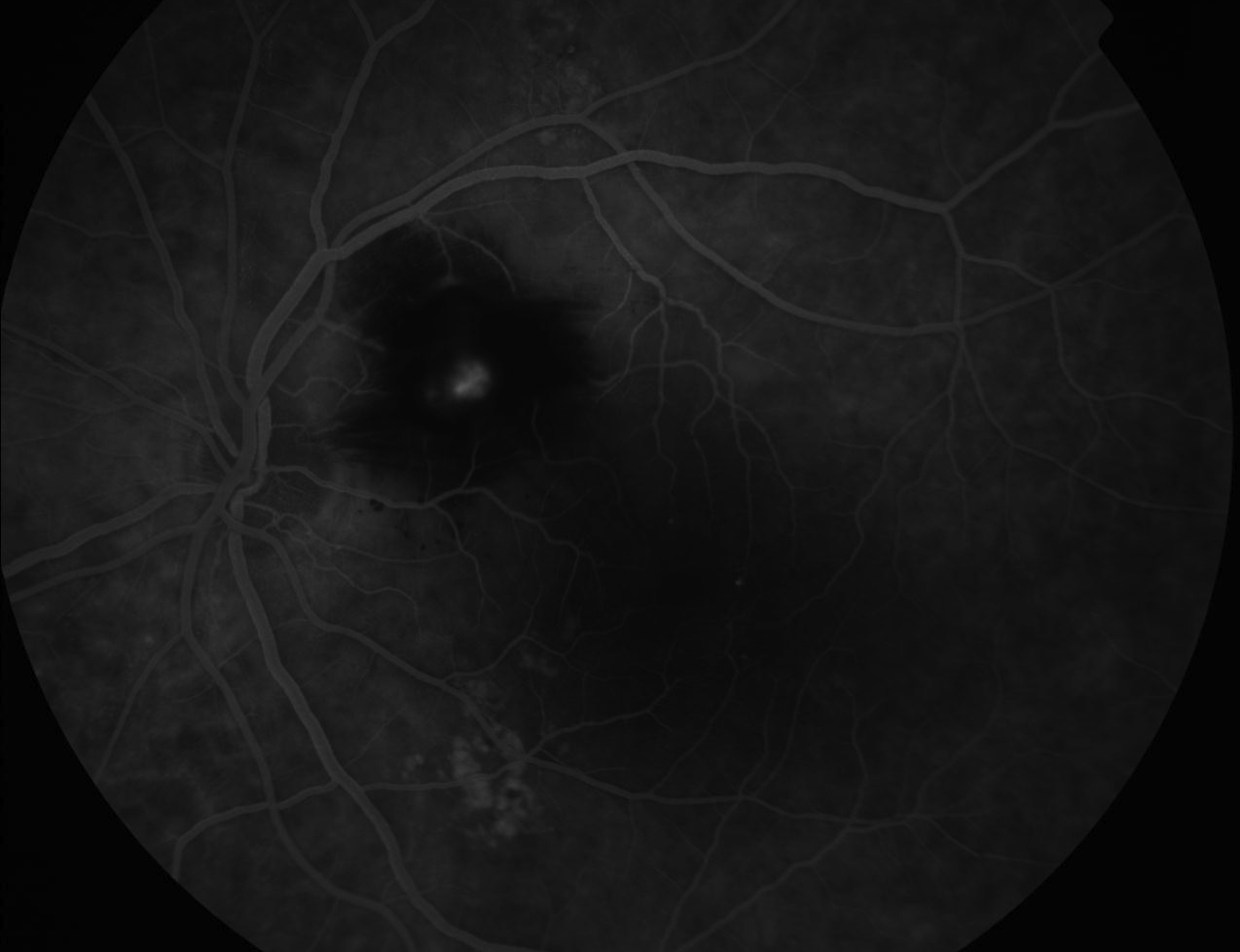
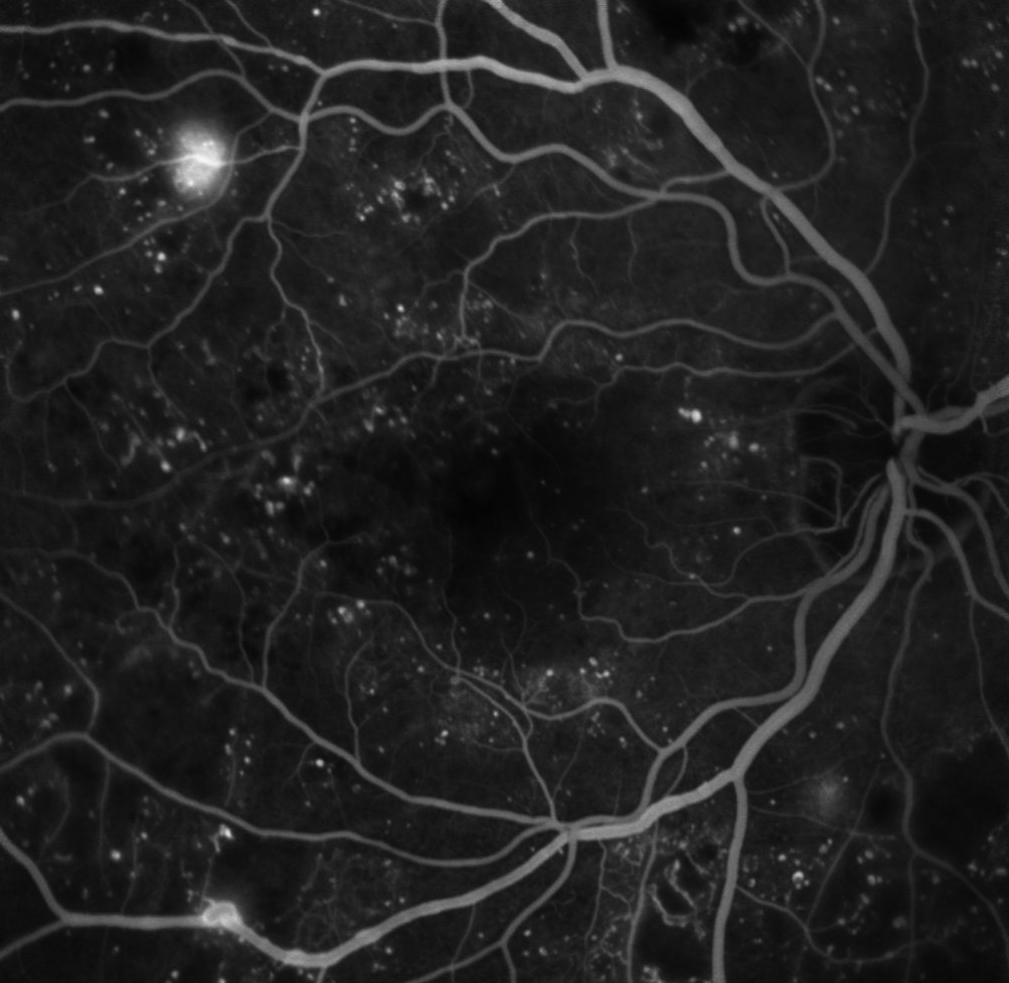
Figure 9.8.13
Neovascularisation of the Optic Disc (NVD)
An extensive fan of new vessels are seen at the disc due to proliferative diabetic retinopathy. Other features include early inferior retinal arcade neovascularisation, laser burns, capillary drop out, subhyaloid haemorrhage, an enlarged foveal avascular zone, and retinal microaneurysms. (55s)
All rights reserved. No part of this publication which includes all images and diagrams may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the authors, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law.
Vitreoretinal Surgery Online
This open-source textbook provides step-by-step instructions for the full spectrum of vitreoretinal surgical procedures. An international collaboration from over 90 authors worldwide, this text is rich in high quality videos and illustrations.
.jpg)
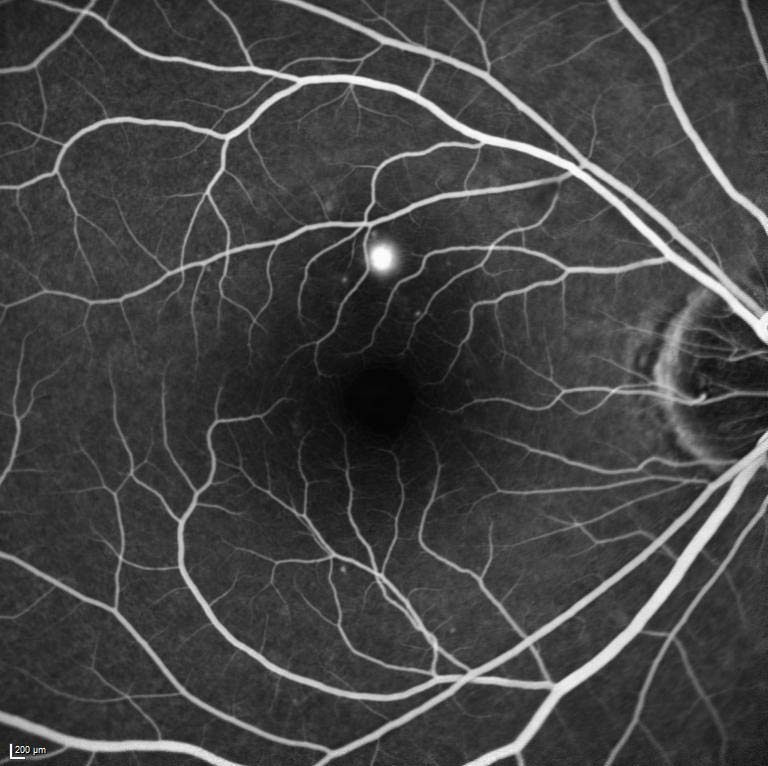
-Choroidal-New-Vessel.jpg)
.jpg)
.jpg)