9 Investigations
9.1 Corneal Topography and Tomography
9.2 Confocal Microscopy
9.3 Optical Coherence Tomography - Macula
9.4 Optical Coherence Tomography Angiography (OCT-A)
9.5 Optical Coherence Tomography - Glaucoma
9.6 Optical Coherence Tomography – Anterior Segment
9.7 Fundus Autofluorescence Imaging
9.8 Fundus Angiography - Fluorescein
9.9 Fundus Angiography - Indocyanine Green
9.10 B-scan Ultrasonography & UBM
9.11 Electrophysiology
9.12 Automated Visual Fields
9.13 Neuroimaging
9.7 Fundus Autofluorescence Imaging
Fundus Autofluorescence (FAF) Imaging is an easy, non-invasive modality for diagnosing retinal disease. It is a modality for metabolically mapping the retinal pigment epithelium (RPE) by identifying naturally or pathologically occurring fluorophores in the posterior segment such as A2-E in lipofuscin granules and minor fluorophores like collagen and elastin. When the pathology is centre-involving, the metabolic changes and loss of RPE corresponds to the level of visual function.
Fluorophores are excited in the blue wavelength (488nm) and emits light in the green spectrum (535 - 580nm) which is then recorded in the yellow-orange spectrum (615 - 715nm). Autofluorescence images are acquired without the administration of any intravenous medication. Both fundus camera and confocal scanning laser ophthalmoscope (cSLO) platforms exist.
FAF imaging is useful to identify retinal pathologies which may not be evident on direct fundus examination or digital fundus photography. Dead RPE appears hypoautofluorescent, as seen dramatically in atrophic age-related macular degeneration (AMD). Diseased or dysfunctional RPE appears hyperautofluorescent. Similar to fluorescein angiography, autofluorescence can also be useful in determining the layer of retinal lesions such as haemorrhage- subretinal bleeding will block underlying RPE hyperautofluorescence, whilst sub-RPE bleeding will not. Pathologies which are typically hypo or hyperautofluorescent are outlined below:
Hypoautofluorescent
- Reduced RPE lipofuscin
- Geographic atrophy
- CHRPE
- Blockage of RPE lipofuscin
- Subretinal haemorrhage
Hyperautofluorescent
- Subretinal hyperautofluorescent material
- Vitelliform lesions (e.g. Best Disease)
- Central serous chorioretinopathy (subretinal fluid)
- Increased RPE lipofuscin
- Fundus flavimaculatus (ABCA4 mutation) flecks
- Pattern dystrophies (RDS/Peripherin mutation)
- Window defect- loss of luteal or photopigment
- White dot syndromes
- Macular telangiectasia type II
- Other
- Optic disc drusen
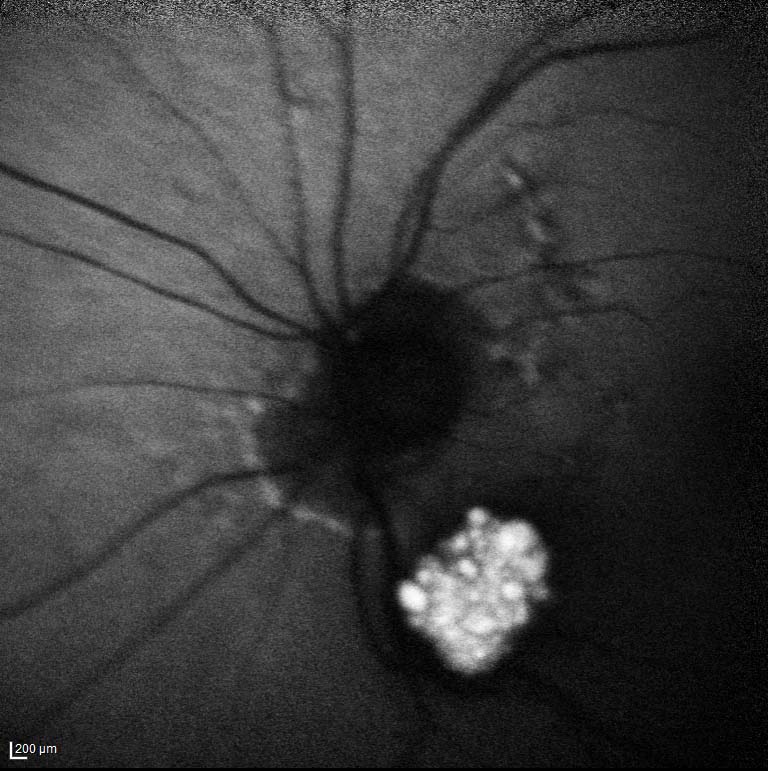
- Astrocytic hamartoma
- Figure 9.7.1: Astrocytic Retinal Hamartoma
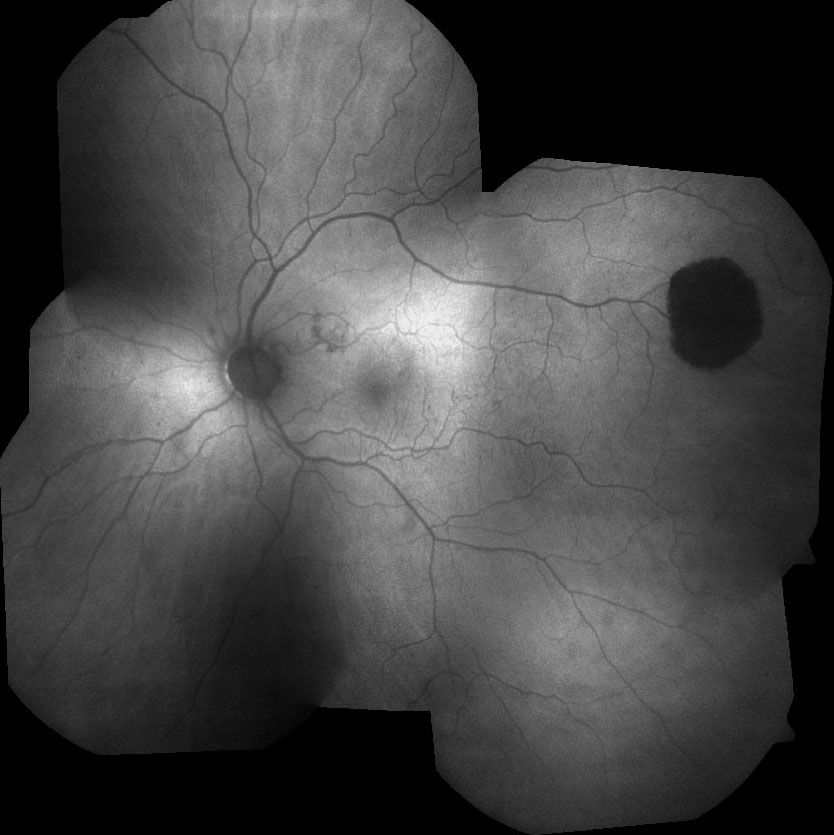
- Figure 9.7.2: Central Serous Chorioretinopathy (Chronic)
- Figure 9.7.3: CHRPE
- Figure 9.7.4: Geographic Atrophy
- Figure 9.7.5: Hydroxychloroquine Maculopathy
- Figure 9.7.6: Macular Telangiectasia (Mactel) Type 2
- Figure 9.7.7: Multifocal Pattern Dystrophy
- Figure 9.7.8: Optic Disc Drusen
- Figure 9.7.9: Vitelliform lesion and Cuticular Drusen
.jpg)
Figure 9.7.2
Central Serous Chorioretinopathy (Chronic)
Blocking of normal retinal autofluorescence is observed centrally. Patchy RPE damage is noted superiorly. The characteristic “waterfall” sign of gravity-dependant shifting of subretinal fluid is demonstrated arising from the inferiotemporal macula.
All rights reserved. No part of this publication which includes all images and diagrams may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the authors, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law.
Vitreoretinal Surgery Online
This open-source textbook provides step-by-step instructions for the full spectrum of vitreoretinal surgical procedures. An international collaboration from over 90 authors worldwide, this text is rich in high quality videos and illustrations.


-Type-2.jpg)
