7 Neuro-Ophthalmology
7.1 Cranial Nerve III (Oculomotor) Palsy
7.2 Cranial Nerve IV (Trochlear) Palsy
7.3 Cranial Nerve VI (Abducens) Palsy
7.4 Cranial Nerve VII (Facial) Palsy
7.5 Optic Nerve Function
7.6 Visual Fields to Confrontation
7.7 Pupils
7.8 Horner’s Syndrome
7.9 Nystagmus
7.10 Neuro-Ophthalmic Differential Diagnoses and Aetiologies
7.3 Cranial Nerve VI (Abducens) Palsy
Cranial nerve VI palsies are extremely common in examinations. Although relatively simple to diagnose, it is important that the examiner look carefully for signs of associated cranial nerve palsies, Horner’s syndrome and papilloedema.
- BO prism - apex points towards the deviation
- Abnormal head position = head turned to the same side
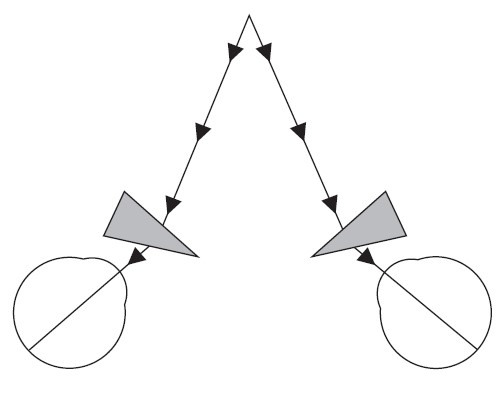
- Hirschberg (Pupil margin = 15°, Iris margin = 30°) - Esotropia
- (Lids normal)
- (Pupils normal)
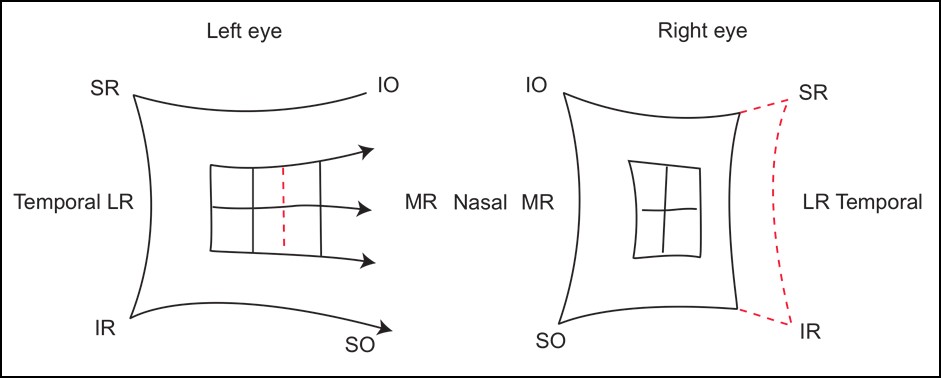
- Esotropia in primary due to the unopposed action of MR
- CTD: ET greater on head turn to opposite side (i.e. incomitant)
- CTN: ET less marked than on CTD (because the eyes converge for near)
- Limitation of abduction due to paralysis of LR
- Slow horizontal abducting saccade
- CN V (Corneal sensation), CN VII, CN VIII
- Look closely for any ptosis or miosis on the ipsilateral side, which localises the lesion to the cavernous sinus
Millard-Gubler syndrome
Ipsilateral CNVI, CNVII+
Contralateral hemiplegia (corticospinal tract)
Foville syndrome
Ipsilateral horizontal gaze palsy (PPRF), CNVII+
Contralateral hemiplegia (corticospinal tract), INO
- Look for papilloedema if there is a bilateral CNVI
- BO prism on affected side
- This would not be done in the exam but can be mentioned
Summary
- Right or left (unilateral or bilateral)
- Isolated or other associated CN palsies / Horner’s syndrome
- Complete vs. partial (assess with ductions, saccades, forced generation, botox to MR)
1. Vascular
Microvascular
HT, Cholesterol, DM, Smoking
Macrovascular
Internal carotid artery aneurysm (cavernous sinus). Subarachnoid haemorrhage, carotico-cavernous fistula, cavernous sinus thrombosis, pituitary apoplexy
2. Neoplastic
- Glioma, meningioma, nasopharyngeal Ca, clivus tumour, chordoma
3. Inflammatory
- GCA, Demyelination, Vasculitis, Sarcoidosis
4. Infective
- HZO, Syphilis, Gradenigo syndrome (mastoiditis or petrositis)
5. Trauma / Surgical
- ↑ ICP (often bilateral), Base of skull fracture
6. Other
- Wernicke
- In children consider: Benign CNVI palsy (usually spontaneously improves after 4-6 weeks), tumour (glioma), ↑ ICP
- ± MRA head with gadolinium
- <50 years
- Other CN palsies (or bilateral) or Horner’s syndrome
- Progressive
- BP, BSL / HbA1C, Lipids (for Vascular risk factors)
- ± ESR / CRP (for GCA)
- ± Vasculitic screen, ACE, Syphilis serology
- ± Tests for Myasthenia
- Hess (right CNVI palsy)
- Contraction of R, expansion of L
- R esotropia (fixation spot deviated nasally)
- R chart: Underaction of LR, overaction of MR
- L chart: Overaction of MR
Treat the underlying cause (e.g. diabetes, hypertension).
Indications for treatment:
- Abnormal head posture
- Diplopia
- Cosmesis
Aims:
- Correct AHP
- Maximise field of BSV
- Align eyes in primary for cosmesis
- Uniocular occlusion for diplopia of the non-dominant eye
- (Fresnel) Prism (BO prism on the affected side)
- Even though incomitant, can be helpful in primary position
- Can only be used if deviation small (e.g. < 30Δ), diplopia in primary
- Botulinum toxin into ipsilateral MR
- Cosmetic improvement, check for complete CNVI
- BUT only temporary, doesn’t improve BSV
- Wait at least 6-12 months and deviation is stable- most will spontaneously resolve
If Partial Paralysis (Aim for Full Field of BSV)
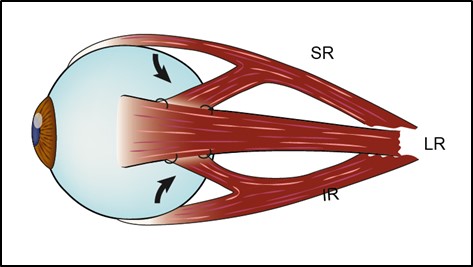
- Recess(MR) / Resect(LR) ± Recess MR of contralateral eye if deviation is very large
If Complete Paralysis (Can’t Cure)
- Transposition (SR / IR to LR) + Botox (recess) ipsilateral MR
- Full tendon transfer (± Foster augmentation modification)
- ½ tendon transfer (e.g. Hummelsheim)
- Jenson procedure (SR / IR split, joined to split LR at the equator)
- Nishida procedure [i] (halves of the SR and IR are sutured onto the sclera)
Nishida Y, Inatomi A, Aoki Y, et al. A muscle transposition procedure for abducens palsy, in which the halves of the vertical rectus muscle bellies are sutured onto the sclera. Jpn J Ophthalmol. 2003;47(3):281‐286. doi:10.1016 / s0021-5155(03)00021-2
Risks
- Anterior segment ischaemia, new vertical deviation, over / undercorrection
- 2nd operation: Contralateral MR Faden suture
All rights reserved. No part of this publication which includes all images and diagrams may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the authors, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law.
Vitreoretinal Surgery Online
This open-source textbook provides step-by-step instructions for the full spectrum of vitreoretinal surgical procedures. An international collaboration from over 90 authors worldwide, this text is rich in high quality videos and illustrations.