4.1 Uveitis Examination
Uveitis patients often appear in clinical examinations. Expect to see low-grade chronic intermediate or posterior uveitis, and the after-effects of previous severe uveitis of any subtype. Acute presentations may be presented as data stations. They are also sometimes used in live examinations if the patient is admitted to hospital at the same time as the examination. The structure of a uveitis examination is similar to anterior and posterior segment examinations, but special attention must be paid to certain aspects once the stigmata of inflammation has been discovered. In general, once you have detected inflammation, ask yourself the following questions:
- What is the age, gender and ethnicity of the patient?
- Is the inflammation acute or chronic?
- Is the pathology unilateral or bilateral?
- Where is the primary site of the inflammation (anterior, intermediate, posterior, panuveitis)?
- Are there idiosyncratic examination features that would narrow the diagnosis?
- Is there evidence of complications and why is the vision reduced?
i. Anterior segment scarring
ii. Vitritis
iii. Glaucoma
iv. Macular oedema
v. Retinal ischaemia and neovascularisation
When asked to summarise your findings, present them in this way – “This 67-year-old man has a left sided panuveitis with evidence of both acute and chronic inflammation. The pattern of chorioretinal scarring is suggestive of toxoplasmosis uveitis. His vision is reduced due to vitritis, but there is no macular oedema. He has evidence of previous retinal vessel occlusion and also glaucoma in this eye, both of which are likely due to his uveitis.”
Attention should always be given to the wording of the question as this will direct you to the primary pathology:
“Examine the…”
- Anterior segment
- Posterior segment
Uveitis patients can have pathology in any part of the eye and the question will not give away the presence of uveitis.
- Always ask for the VA and IOP. In acute uveitis the IOP is often low, although there are exceptions causing hypertensive uveitis (e.g. herpetic). In chronic uveitis the IOP is often high and can be due to open angle (e.g. the uveitis itself, steroid response) or closed angle mechanisms (e.g. pupil block from peripheral anterior synechiae or posterior synechiae).
- Always stand back and examine the patient as a whole. Age, gender and ethnicity are extremely important in narrowing the potential differential diagnoses. Does the patient have any skin rashes, vitiligo, poliosis or tattoos? Note the presence of hearing aids (VKH, Cogan’s syndrome) or visual aids. Iris heterochromia is more obvious from a distance. Note if the eyes are macroscopically inflamed (red) before proceeding but resist describing this as “conjunctivital injection” as it may be scleritis or episcleritis.
- Symblephara, ankyloblepharon, forniceal shortening are often more obvious on gross inspection before beginning the slit lamp examination
i. Conjunctiva and Sclera
Comment on any injection and determine the ocular layers involved. Conjunctival injection shows fine, dilated vessels that move freely over the ocular surface, without a particular orientation. Episcleral vessels can be seen below the conjunctival vessels and are oriented radially. Scleral injection is deep red / purple discolouration of the sclera. If any are noted, suggest a phenylephrine test – 2.5% phenylephrine should blanch the conjunctiva only, while 10% should blanch both conjunctival and episcleral vessels. Neither will blanch scleral vessels
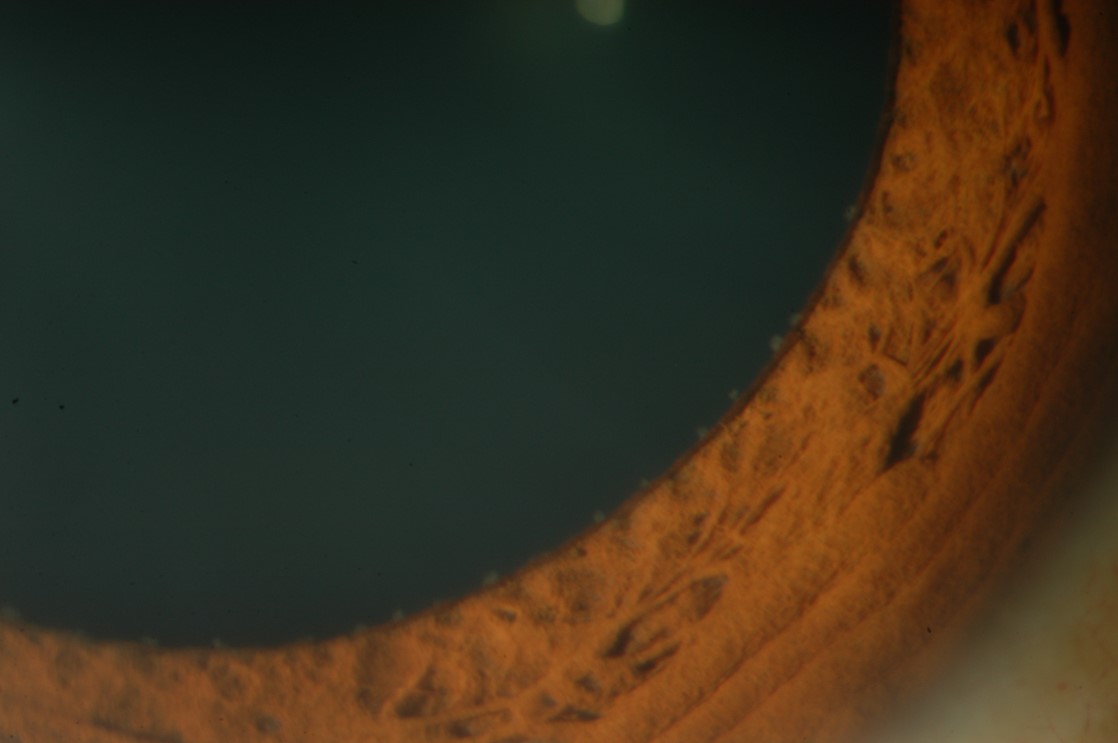
ii. Cornea
Note the presence of band keratopathy signifying chronic uveitis. Examine carefully for keratitis precipitates (KP). Note their character and distribution (e.g. Arlt’s triangle vs pan-corneal). Pan-corneal KP suggest an infective aetiology (including syndromes newly recognised as having a viral association or aetiology, such as Fuch’s uveitis syndrome and Possner-Schlossman syndrome). Changes may be more visible with retro-illumination
iii. Anterior Chamber (AC)
Cells and flare are the primary finding. Grade the number of cells with a 1x1mm slit beam at 45 degrees
Cells
0
< 1 cell
0.5
1 – 5 cells
1 +
6 – 15 cells
2 +
16 – 25 cells
3 +
26 - 50 cells
4 +
50 cells
Flare
0 +
None
1 +
Faint
2 +
Moderate (iris and lens detail clear)
3 +
Marked (iris and lens detail hazy)
4 +
Intense (plasmoid or fibrinous aqueous)
iv. Iris
- Look for Koeppe (pupil margin) and Busacca (mid iris) nodules which suggest granulomatous uveitis (e.g.. sarcoidosis, TB, toxoplasmosis)
- Iris transillumination defects are suggestive of herpetic viral infection
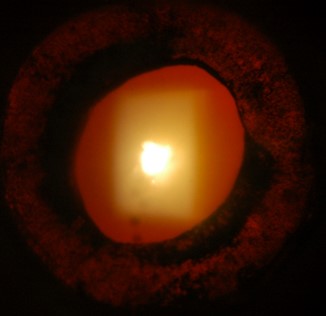
v. Lens
Note the presence of cataract and its type. Cataract may be present due to inflammation or its treatment with steroids. Comment on position of any posterior synechiae, e.g. 3-9 oclock. If an intraocular lens (IOL) is present, note capsular adhesions and opacification.
vi. Anterior Vitreous
Grade cells in the anterior vitreous the same as in the AC by pushing the slit lamp beam posterior to the lens. Note the colour of cells – brown pigmented cells suggest old inflammation, whereas white cells are generally acute. These are finer and more uniform than the tobacco dust (Shafer’s sign) from a retinal break or tear and are not the same as red cells from vitreous haemorrhage. Atypical large cells may indicate vitreous lymphoma or chronic endophthalmitis.
All rights reserved. No part of this publication which includes all images and diagrams may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the authors, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law.
Vitreoretinal Surgery Online
This open-source textbook provides step-by-step instructions for the full spectrum of vitreoretinal surgical procedures. An international collaboration from over 90 authors worldwide, this text is rich in high quality videos and illustrations.