5.1 Ectropion
Introductory Comments
Candidates should direct their examination towards determining the:
- Cause of the ectropion
- Potential surgical options to address the ectropion
- Whether any exposure keratopathy is present
Most ectropion cases in examinations (and clinical practice) will involve the lower lid. Upper lid ectropion is very rare and is usually due to floppy eyelid syndrome and eyelid laxity. Involutional upper lid ectropion can present with punctal ectropion. Cicatricial upper lid ectropion is exceedingly rare.
The remainder of this chapter will deal with lower lid ectropion.
This is relevant for determining severity of exposure keratopathy as well as the viability of certain surgical repair options (such as prolonged surgical closure of the lids).
Stand back from the patient and observe for a few seconds, then advance closer and continue to observe. While observing comment on the features mentioned below:
- Ectropion: Generalised, Medial, Lateral, or Tarsal (complete eversion of tarsal plate)
- Punctal position: Normal punctal position is directly below / slightly lateral to upper punctum, facing the tear lake
- Inferior scleral show
- Conjunctival injection
- Severe epiphora from punctal stenosis: A patient will usually present with a tissue paper in one hand on inspection and a visibly raised tear film height
- Gently rub the patient’s ipsilateral cheek or have the patient open their mouth which will confirm a cicatricial component
- Scars / masses (suspicious for malignancy or previous surgery)
- Look for upper lid dermatochalasis which can be used as a skin graft donor site
Pull the lower lid down and ask the patient to look up. Observe the inferior fornix. Then ask the patient to look down. Observe the tarsal plate and fornix for movement.
- A tarsal ectropion (frank eversion of the tarsal plate) can indicate dehiscence or severe attenuation of the inferior retractors and their insertion to the lower tarsal plate. In less severe ectropion the presence of retractor dehiscence is suggested by:
- Deepening of the inferior fornix
- Visible separation of retractors from the tarsal plate (a red area between the white band of the retractors and the inferior tarsus)
- Lack of movement of the distracted lower lid with downgaze
Generalised Lid Laxity
Distraction and “Snap back” test: Pull the lower lid directly away from the globe and observe how far it can be distracted (> 8 - 9mm is considered “abnormal”) and how quickly it “snaps back” onto the globe when released. A normal eyelid does not require a blink to reposition itself on the globe
Lateral Canthal Tendon (LCT) Laxity
Note any rounding of the lateral canthus. Pinch the lower eyelid and pull medially (“Medial distraction test”). Medial distraction of the lateral canthus > 2mm is abnormal. Compare with the contralateral side
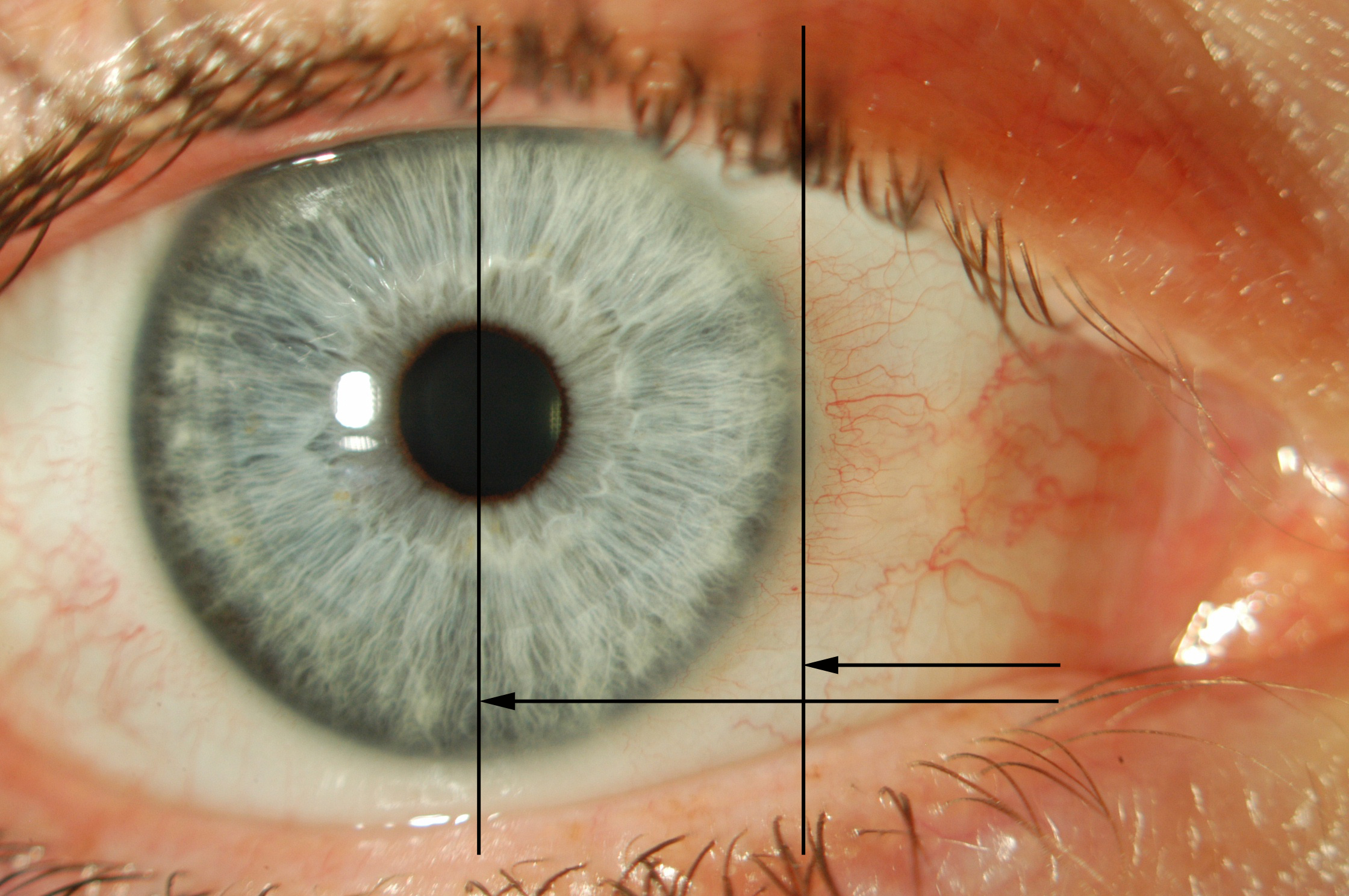
Medial Canthal Tendon (MCT) Laxity [i]
There is no universally agreed grading system for MCT laxity. Readers are encouraged to refer to Olver et. al. Lower Eyelid Medial Canthal Tendon Laxity Grading. Ophthalmology. 2001 Dec;108(12):2321-5.
Note the resting position of the punctum. Pinch the lower eyelid and pull laterally (“Lateral distraction test”)
- “Moderate”: Punctum reaches limbus
- “Severe”: Punctum reaches pupil – (stabilisation of the MCT may be required)
Paralytic ectropion is usually obvious. Recovered CNVII palsy can still cause ectropion and can be subtle. The most sensitive finding is orbicularis weakness
This is most important, particularly in facial nerve palsy cases. Check for:
- Bells phenomenon
- Firmly but gently grip both upper eyelids with your thumbs to prevent closing. Ask the patient to “Close your eyes”. With an upward Bells phenomenon, the globes rotate up and out
- Orbicularis strength
- Ask the patient to close their eyes as tightly as possible, then try to force them open. You will not be able to overcome the normal orbicularis muscle power
- Lagophthalmos
- Ask the patient to “Rest your head back and gently close your eyes as if you are going to sleep”. Assess whether there is an opening between the upper and lower eyelids- if so, measure this with a ruler
- Corneal sensation
- Ask the examiner for this- under examination conditions you will usually be told the result.
- Punctate corneal epithelial erosions
- Inform the examiner you would check with fluorescein and the slit lamp for this sign of dry eye
Comment on:
- Punctal position of the punctum relative to the tear lake
- Punctal stenosis (a punctal 3-snip procedure may have to be performed at the time of surgery)
- Inferior Conjunctival inflammation
- Suspicious skin or lid margin lesions (exclude malignancy)
If epiphora is the major complaint, mention that you would also like to assess patency of the lacrimal system with a Jones test and syringing. It is common for ectropion and lacrimal system obstruction to co-exist. Suspicious skin lesions should be biopsied.
Summary
- Right or left
- Involutional / cicatricial / paralytic ectropion
- ± Generalised or medial / lateral, Tarsal
- ± Horizontal lid laxity
- ± Exposure Keratopathy
Congenital
This is rare and usually due to skin shortage i.e. anterior lamellar cicatrix)
Acquired
Involutional
Cicatricial
Paralytic
Mechanical

Involutional
Aetiology: Aging (weakness of pretarsal orbicularis oculi)
1. Lower lid retractor laxity
2. Horizontal lid laxity
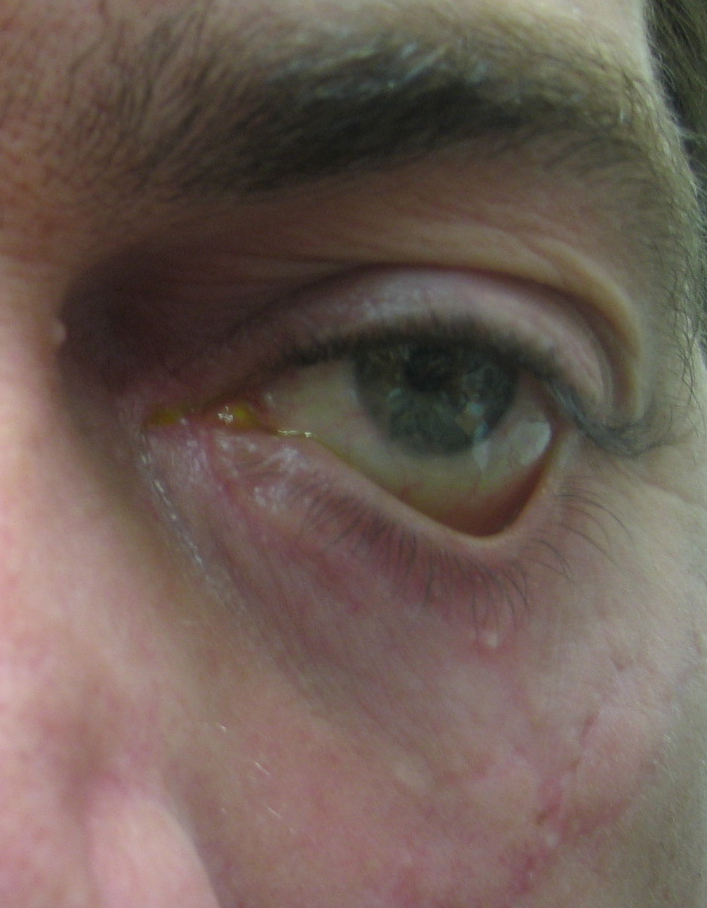
This picture demonstrates a tarsal ectropion with complete eversion of the tarsal plate. The exposed conjunctiva becomes inflamed.
Mechanical
Aetiology: Mass lesion
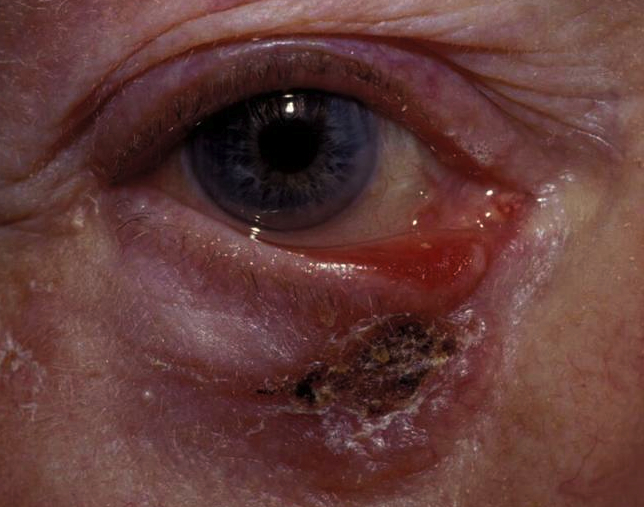
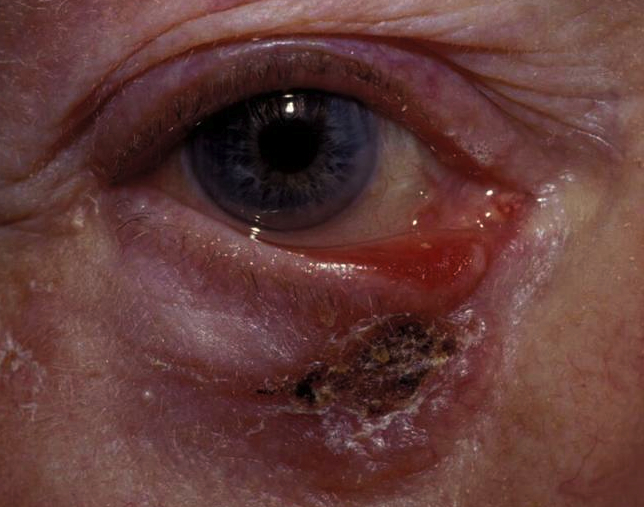
This photograph demonstrates a combined mechanical / cicatricial ectropion and due to a skin cancer. Excision with histologically clear margins should be performed prior to reconstruction.
Cicatricial
Aetiology: Actinic, surgery, trauma, burns, dermatitis / rosacea / HZO
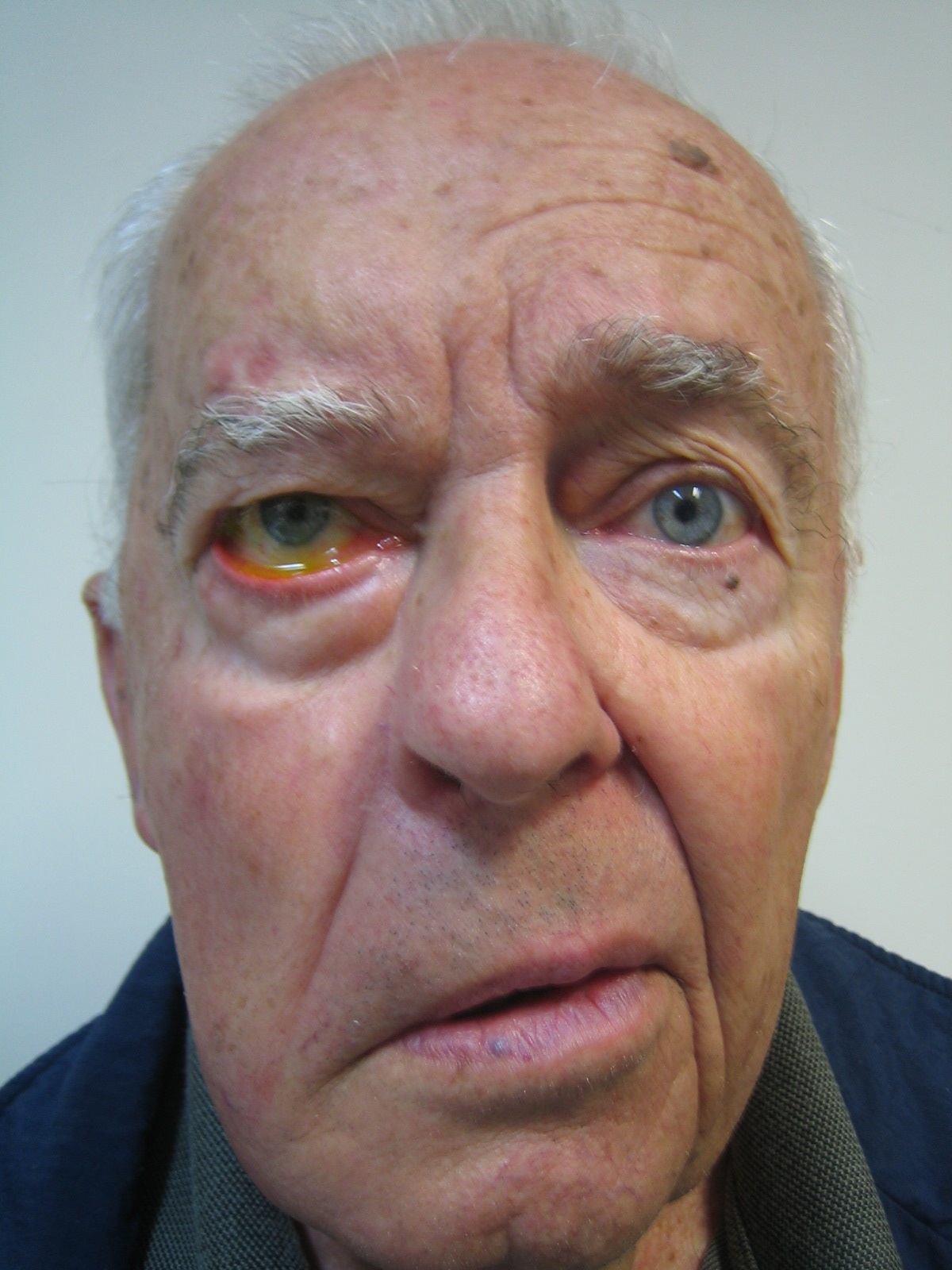
Paralytic
Aetiology: CN VII palsy (these also have a mechanical element due to the weight of the mid-face pulling the lower lid inferiorly)
Involutional
Aetiology: Aging (weakness of pretarsal orbicularis oculi)
- Lower lid retractor laxity
- Horizontal lid laxity
This picture demonstrates a tarsal ectropion with complete eversion of the tarsal plate. The exposed conjunctiva becomes inflamed.

Mechanical
Aetiology: Mass lesion
This photograph demonstrates a combined mechanical / cicatricial ectropion and due to a skin cancer. Excision with histologically clear margins should be performed prior to reconstruction.
All rights reserved. No part of this publication which includes all images and diagrams may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the authors, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law.
Vitreoretinal Surgery Online
This open-source textbook provides step-by-step instructions for the full spectrum of vitreoretinal surgical procedures. An international collaboration from over 90 authors worldwide, this text is rich in high quality videos and illustrations.