7 Neuro-Ophthalmology
7.1 Cranial Nerve III (Oculomotor) Palsy
7.2 Cranial Nerve IV (Trochlear) Palsy
7.3 Cranial Nerve VI (Abducens) Palsy
7.4 Cranial Nerve VII (Facial) Palsy
7.5 Optic Nerve Function
7.6 Visual Fields to Confrontation
7.7 Pupils
7.8 Horner’s Syndrome
7.9 Nystagmus
7.10 Neuro-Ophthalmic Differential Diagnoses and Aetiologies
7.7 Pupils
The pupil station appears frequently in examinations. Candidates should remember that there can only be two problems with pupils:
- “Sensory” problem
- Problem with pupillary light response
- Relative Afferent Pupillary Defect (RAPD).
- Pupils equal
- “Motor” problem
- Anisocoria
The rest of the pupillary examination is then tailored according to whether a RAPD or anisocoria is present. If anisocoria is present, it is essential to determine which eye has the pathological pupil. Anisocoria worse in dark implies pathology of the smaller pupil (which is not dilating). Anisocoria worse in light implies pathology of the larger pupil (which is not constricting).
Begin with the room lights on.
- Remember that visual acuity may be normal despite a marked RAPD
- Size (Anisocoria > 1mm = non-physiological)
- Shape (beware of trauma, iris atrophy, posterior synechiae and a prosthetic eye!)
- Heterochromia iridis (Horner’s syndrome)
- Ptosis (paralysis of Müllers muscle or Levator palpabrae superioris)
- Inverse ptosis (lower lid elevation in Horner’s)
- Strabismus (e.g. CN III palsy)
- Scars (neck scar with Horner’s, tracheostomy scar with previous trauma)
- Ask the patient to fixate on a distant point (ensuring that your head is not in the way) so that they do not accommodate
- Use a pupil diameter measuring ruler, which is easier to read than the graticule on a ruler
Although the size of the pupils can be documented in millimetres, it is the relative change in anisocoria in light and dark which is more important than the absolute values.
- Measure pupils in light
- Measure pupils in dark
- Ask the examiner to switch the room light off (usually there will be a lamp in the room so that there is still some ambient light). If possible, avoid using a pen torch to view the pupils- it is difficult to shine this evenly in both eyes and defeats the purpose of inspecting pupils in dark. Unfortunately, inspecting pupils in dark is always difficult in patients with dark iridae. It is important to measure the pupils quickly once the room lights have been turned off. Patient’s with Horner’s syndrome have a dilatation lag - the affected pupil will dilate more slowly by passive relaxation of the sphincter pupillae alone, compared to the fellow eye with intact dilator pupillae activity
Anisocoria worse in dark implies a problem with the smaller pupil (not dilating).
Anisocoria worse in light implies a problem with the larger pupil (not constricting)
Physiological Anisocoria:
- Anisocoria < 1mm
- Anisocoria same in light and dark
- Normal light reaction
- No other neurological signs
- Pupillary reflexes are best observed whilst the room lights are still dimmed
Shine the light in the right eye and note:
- Direct light response (right eye)
- Consensual light response (left eye)
- Then repeat with the other (left) eye. For the consensual reflex it may be easier to look at the contralateral pupil dilating after removing light from the ipsilateral side
- Sluggish direct and consensual reflexes indicates a parasympathetic problem (problem with constriction)
- A sluggish direct reflex with a normal consensual reflex indicates an optic neuropathy
- A bright, uniform light source (direct or indirect ophthalmoscope) should be used (not a pen torch). It is important that the light pauses on each pupil before “swinging” quickly to the contralateral eye
- Ask the patient to fixate on a distant target (focusing on a close target will activate the accommodation reflex)
- Shine the light in the right eye. Count in your head “one one thousand, two one thousand”
- Quickly swing the light to the other (left) eye. Preferably this should be below the line of sight of the patient to prevent accommodation, and with the light directed towards the nasal retina (since there are slightly more crossed than uncrossed neurones). However, these preferences should not delay the speed of the “swing”, which needs to be rapid
- Observe for an initial dilation of this eye (i.e. a RAPD)
A RAPD can be graded:
- Grade 1: A weak initial constriction and greater redilatation. Any asymmetry between the two eyes is significant
- Grade 2: Initial stall and greater redilation
- Grade 3: Immediate pupillary dilatation
- Grade 4: Immediate pupillary dilatation following prolonged illumination of the good eye for 6 seconds
- Grade 5: Immediate pupillary dilatation with no secondary constriction
- The presence of a RAPD implies a sensory problem (involvement of the afferent pupillary light pathway- usually the retina or optic nerve). For it to occur there needs to be asymmetry between the two eyes. If both afferent light pathways are equally affected, a RAPD will not be present. RAPDs do not occur with dense cataracts, vitreous haemorrhages and most cases of amblyopia (occasionally it may subtly occur in dense amblyopia). Unconscious patients can be tested for a RAPD. RAPDs can be objectively graded (in log units) by placing neutral density filters over the normal eye until the RAPD has been neutralised, but this is unlikely to be expected of examination candidates due to time constraints
- Even if a pupil is known to be pharmacologically dilated or non-reactive, the presence of a “reverse RAPD” can be examined by comparing the direct and consensual reflexes in the good eye
- Light-near dissociation is defined as a diminished pupillary light reflex with relative sparing of the accommodation response
- This only needs to be tested if the light reflex is abnormal (if the light reflex is normal the near reflex will nearly always be normal). Despite this, some examiners may wish the candidate to check for a near pupil response in all patients. The light reflex passes through dorsal midbrain, whilst the near reflex passes through ventral midbrain
- Ask the patient to place their thumb in front of the face
- Ask the patient to “Look at a distance target”
- Ask the patient to “Look at your thumb”. Do the pupils constrict (more than with light)?
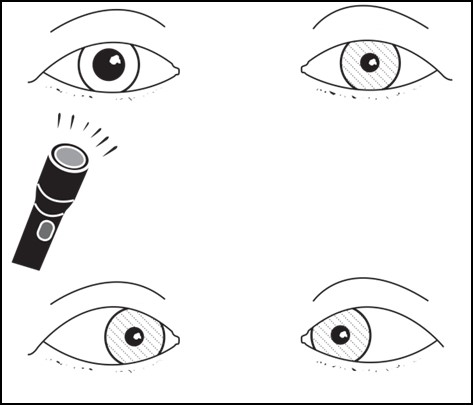
Figure 7.7.1
Light-Near Dissociation
The pupil contricts when focusing on a near object but not when light is shone into it.
- In the presence of RAPD (sensory)
- Perform a full optic nerve exam
- Check extra-ocular motility (in case of orbital apex or cavernous sinus syndrome)
- In the presence of aniscoria (motor)
- Check extra-ocular motility (in case of CN III Palsy)
- Perform a full optic nerve exam
- Slit lamp examination
- Posterior synechiae, trauma
- Signs of syphilitic uveitis: Interstitial keratitis, iris atrophy, chorioretinitis, papillitis, uveitis
- Vermiform movements (Adie’s tonic pupil)
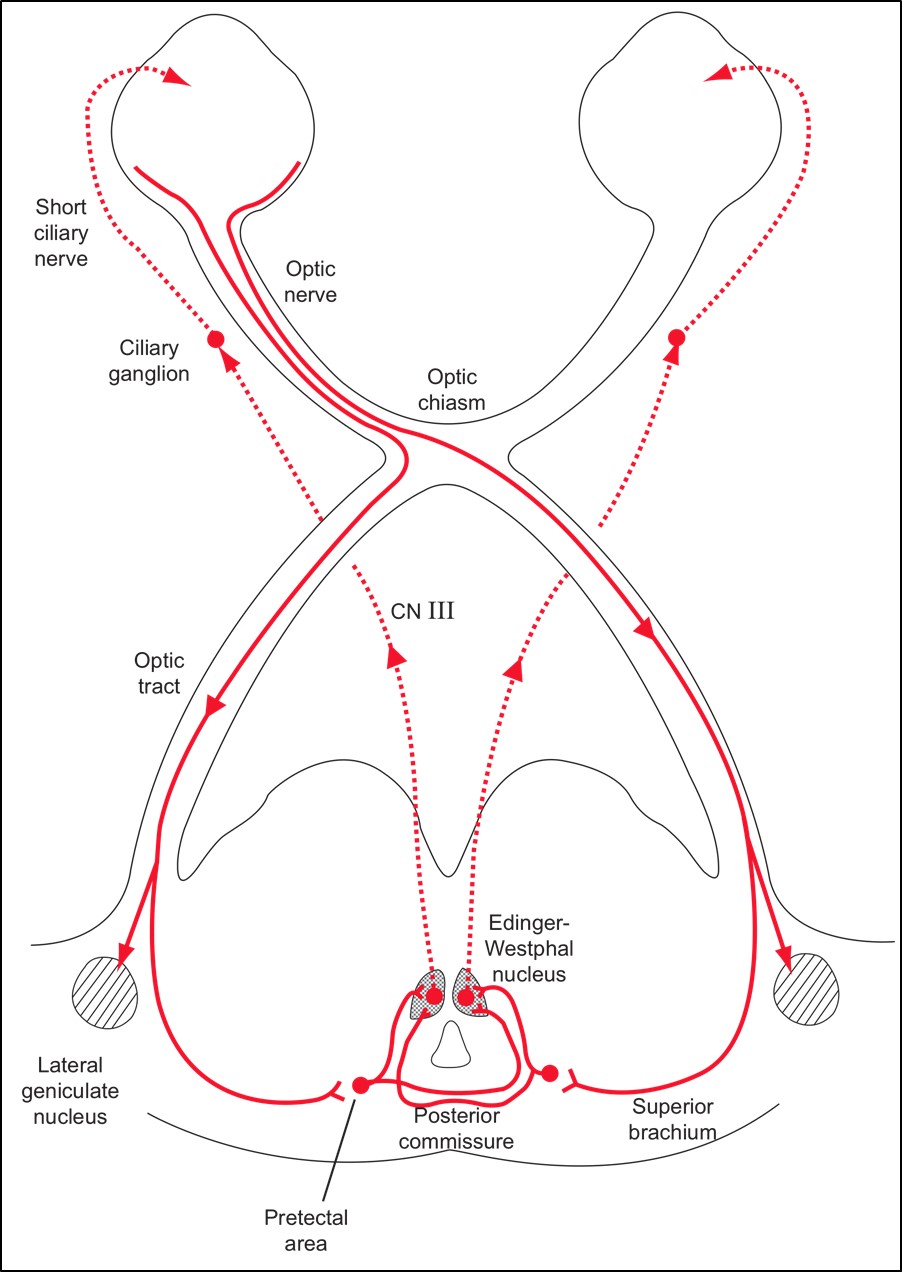
The pathway of the light reflex should always be remembered:
Light Near Dissociation
(Mnemonic: “ABCD”)
- Adie’s pupil, Argyl Robertson Pupil, Alcohol
- Bilateral severe loss of afferent input into both eyes (retinal / optic nerve, optic chiasm pathologies)
- CN III palsy with aberrant regeneration
- Dorsal Midbrain Syndrome (Parinaud’s syndrome)
Anisocoria Worse in Light
(Mnemonic: “4Ts”)
- Trauma
- Third nerve
- Tonic (Adie’s)
- Tropicamide (Pharmacological dilation)
Anisocoria Worse in Darkness
(Mnemonic: “4Ps”)
- Pilocarpine (Pharmacological miosis)
- Prostitute (Argyl Robertson pupil due to neurosyphilis)
- Pancoast (Horner’s syndrome)
- Posterior Synechiae
Adie’s Tonic Pupil
Epidemiology
Young women
Natural History
Initially a large pupil which becomes small after several years
Must Rule Out
Syphilis, Diabetes, GCA, VZV, Dysautonomia (familial, HIV)
Clinical Features
- Slow (tonic) re-dilation after accommodation effort
- Sectoral palsy on constriction
- Vermiform movements at the pupil border on constriction
- Light near dissociation – occurs after 8 weeks
Investigation
- Instil Pilocarpine 0.125% into both eyes and the affected pupil will constrict.
Rationale: Denervation hypersensitivity (which occurs after 1 week) - If the pupil does not constrict, apply Pilocarpine 1%.
This will constrict a CNIII palsy but not pharmacological mydriasis
Systemic Issues
Reduced deep tendon reflexes (e.g. ankle jerk), 70% of Holmes-Adie Syndrome
Anhidrosis (Ross syndrome), hyperhidrosis
Postural hypotension, cardiac arrhythmias
Epidemiology
Older men
Associations
Tertiary Syphilis; Diabetes; Alcohol
Clinical Features
- Small pupils (damage to corticotectal fibres inhibitory to the Edinger-Westphal nucleus → pupilloconstrictor tone)
- Light-near dissociation
- ± Interstitial keratitis, iris atrophy, chorioretinitis, papillitis, uveitis (syphilis)
Investigations
Check syphilis serology (± lumbar puncture), BSL
Adie’s Pupil
(Vermiform movements; Sectoral Constriction; Slow Constriction & Re-dilation)
Argyll Robertson Pupil
Epidemiology
Adie’s Pupil
Young & Female
Argyll Robertson Pupil
Old & Male
Uni / Bilateral
Adie’s Pupil
Unilateral (80%); (20% are bilateral → investigate for Syphilis or vasculitis)
Argyll Robertson Pupil
Bilateral
All rights reserved. No part of this publication which includes all images and diagrams may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the authors, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law.
Vitreoretinal Surgery Online
This open-source textbook provides step-by-step instructions for the full spectrum of vitreoretinal surgical procedures. An international collaboration from over 90 authors worldwide, this text is rich in high quality videos and illustrations.