6 Strabismus
6.1 Eye Movements Examination
- Sit on the right of the patient, your eyes and the patient’s eyes should be at the same level
- Speak whilst examining
- Ask children their age
- Look around the room for clues – spectacles, parents (for inherited syndromes)
The worse eye is usually the affected one (may be amblyopic)
It is easiest to estimate the script of spectacles by comparing the image of a line viewed through the lens and just around it. A distance line such as a doorway is perfect for this purpose.
Hand Neutralise
Minus lens → “With” movement
Plus lens → “Against” movement
Astigmatism
Ground in Prism
The image of the line through the lens has a fixed deviation away from the image of the line just around it. This cannot be compensated by moving the lens. The apex of the prism points towards the deviation.
Fresnel Prism
Method for easy check: turn spectacles side-on
BO (CNVI palsy), BD (CNIV palsy on affected eye)
- Have the patient fixate on a distant target- choose one line above their visual acuity
- Only comment on a strabismus if it is obvious (say “there appears to be an exo or eso deviation” in case the patient has a dragged macula and there is no tropia)
- Ask patient to “Please sit up straight” and stand back to inspect
- Face turn? In direction of action of paretic muscle
- Chin up / down? Up in elevator paresis, Down in depressor paresis
- Correct any AHP before cover tests (check for neck pathology)
Shine a pen torch into the patient’s eyes and inspect the corneal reflexes. In patients with straight eyes, they should be symmetrical and lie over the same point on the cornea. In patients with strabismus, the corneal reflex of the fixing eye will lie centrally within the pupil, and the other will be displaced (1mm of corneal decentration = 15 Δ strabismus, Pupil margin = 30 Δ, Limbus = 90 Δ). Be aware that tropias can only be definitively diagnosed with cover testing. The Hirschberg test becomes more important when vision is poor (e.g. < 6 / 60 in either eye) and cover-testing is not possible.
5. Globe Position
Proptosis (axial vs. non-axial)
6. Other
Nystagmus, facial asymmetry, hearing aids, scars (conjunctiva- squint surgery)
7. Ask Yourself
“Could this be TED?”- proptosis, chemosis, injection, lid retraction
- Ensure the patient can fixate “Tell me if I block your view”
- If VA <6 / 60 can’t do cover! → Perform Hirschberg (corneal light reflexes) and / or Krimsky (corneal light reflexes through prism placed over the fixing eye) tests.
- The patient should wear their distance (& near) spectacles (unless they have prisms!)
- This helps the patient if they can’t fixate on a target uncorrected
- It is crucial in accommodative esotropia to test with and without spectacles
- Cover for tropia (manifest)
- Uncover for phoria (latent)
- Perform cover, uncover tests slowly (hold the cover in place during the cover test for an adequate period of time). Speak out loud “On covering the right eye, there is a small / moderate / large left esotropia”. A tropia may be unilateral or alternate between eyes (fixation switches after each cover). During cover testing, look closely for latent nystagmus and / or dissociated vertical deviation (DVD). The uncover test is only useful if the cover test has demonstrated orthotropia in the other eye
- Alternate Cover for Tropia & Phoria
- Perform alternate cover tests with fast “switch” (then pause) to break fusion
Cover-test Distance (CTD) in Primary
- If vertical deviation / height (“R over L” or “L over R”; hyper / hypotropia if 1 eye fixing) and possible CNIV palsy → Perform Parks 3 step test
- If horizontal deviation in primary and possible CNVI palsy → Check for incomitance in left / right gaze
- ± Chin up / down for alphabet patterns (“V” pattern think of: Browns, IOOA, bilateral CN IV palsy). Ask yourself where the eso or exo is worst:
- Eso deviation worst (points to apex of letter) in chin-up (downgaze) = V pattern
- Exo deviation worst (points away apex of letter) in chin-up (downgaze) = A pattern
Cover-test Near (CTN) in Primary
- You must use a good accommodative target (not a finger, light)
- ± Reading add
Notes on Cover-Testing
- Cover the fixing eye first
- A freely alternating tropia suggests similar visual acuity in both eyes
- When checking for incomitance, only do alternate cover test (not cover, uncover). Keep the patient dissociated by keeping one eye covered at all times
- Prism cover test:
- Cover the deviating eye with a prism & cover, move the paddle to cover the fixing eye, increase the prism until there is no longer refixation
- When measuring CTN with prism, get the child to hold the target on your nose or put a small sticker on your nose!
- When measuring DVD, place prism apex up in front of the affected eye
Either a fixation target or a pen torch may be used. A pen torch has the advantage that corneal reflexes can be viewed but some examiners don’t like this technique. Unlike cover testing for near, accommodation doesn’t have to be controlled. Gently hold your hand out near the patient’s chin or forehead (this “reminds” the patient to keep their head still) and make your movements slow but deliberate (avoid multiple passes). The upper eyelids may need to be elevated when the patient is in downgaze.
- Horizontal pass (twice)- watch lids / pupils for aberrant regeneration / Duane
- “H” pattern
- ± Straight up / down (thyroid eye disease TED, A/V patterns)
- ± Convergence
Notes on Ocular Rotations
- You must know which eye is fixing
- Grading: - 8 (eye looking in opposite direction to attempted extreme gaze) → - 4 (eye looking in primary on attempted extreme gaze) → 0 (normal)
- Say “- 2 defect of elevation in abduction…”, not “restriction” (unless you have demonstrated this first)
- Check ductions (cover the contralateral eye) if there is a defect (goes further if palsy is present, unlike restriction)
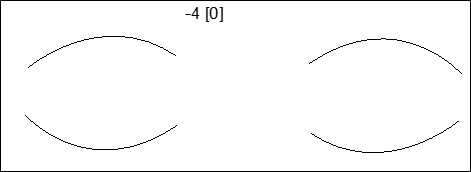
- Record versions and ductions (in square brackets) e.g. - 4[0]
- For all muscles other than the medial / lateral rectus, look for a vertical movement on cover testing at extremes of gaze
- An up / down movement on attempted horizontal movement is an “up / downshoot”
- For SR / IR, SO / IO over / underaction look for vertical movement when alternate cover testing at the ends of the “H”
- You can only say “there is suggestion of e.g. IOOA” prior to performing an alternate cover test
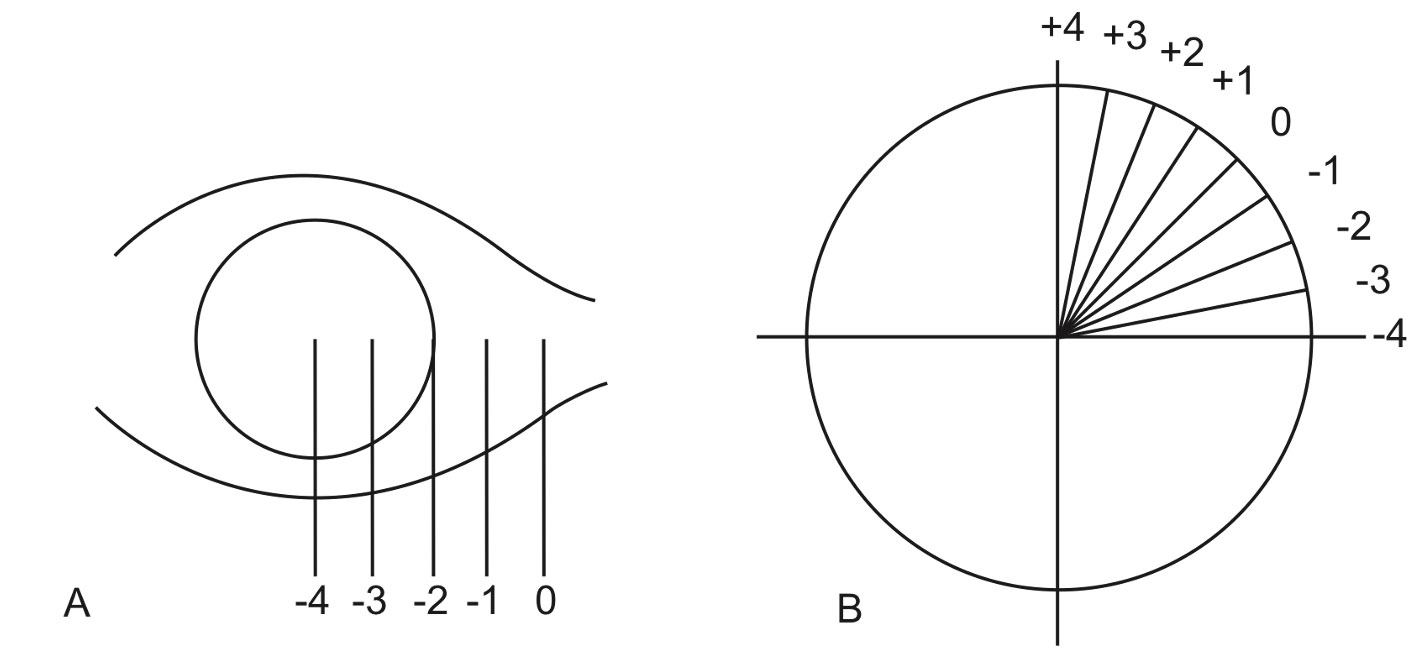
Figure 6.1.1
Grading and Documenting Ocular Rotations
A: Grade 0 is normal. For horizontal versions a grade of -4 indicates that the eye remains in primary when attempting to fully abduct or adduct.
B: When testing ocular movements at the extreme corners of gaze (at the ends of the “H”), +4 indicates overaction to vertical, -4 indicates underaction to horizontal).
C: The two eyes are drawn and points of gaze are graded.
- Test monocularly (easier to inspect one eye at a time)
- Use finger & pen ~20cm apart in field of expected deficiency. Don’t “wiggle” the targets
i. Normal (Fast)
- Occurs in restrictive disease up to the point of restriction
ii. Abnormal
- Occurs in neurological and myogenic disease:
Hypometric
- “Undershoot”
- Generalised slow saccades occur in supranuclear palsy (Parinaud- worse up, progressive supranuclear palsy PSP- worse down), CPEO and myaesthenia gravis (“intra-saccadic fatigue”)
- Uni-directional slow saccades occur with CN palsies and INO
Hypermetric
- Cerebellar Disease
Children
- Retinoscopy
- Fundoscopy
- (Stereopsis)
Adults
- Prism cover test (see above)
- Prism subjective test
- Predict post-operative diplopia by putting up a prism
- Myasthenia Gravis
- Cogan’s lid twitch, fatigueability, orbicularis strength
- Pupils
- CNIII palsy, Light near dissociation in Parinaud (normal in MG)
- Optokinetic Nystagmus (OKN)
- Retraction nystagmus in Parinaud. Ask the patient to “Count the lines as I move the tape” (down)
- Doll’s head / Bells
- Abnormal in CPEO
- Normal in supranuclear palsies (e.g. Parinaud, PSP)
- Forced duction
- Restriction (TED, Orbital fracture, Myositis, Cancer, Browns, CFEOM)
- Fundoscopy
- Papilloedema (CNVI palsy)
- Maddox Rod
- CNIV palsy for excyclotorsion (> 10° if bilateral)
- Vertical fusion
- Increased in congenital CNIV palsy, TED (long-standing)
- Ask for a Hess test
Previous
6.0 Introduction
All rights reserved. No part of this publication which includes all images and diagrams may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the authors, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law.
Vitreoretinal Surgery Online
This open-source textbook provides step-by-step instructions for the full spectrum of vitreoretinal surgical procedures. An international collaboration from over 90 authors worldwide, this text is rich in high quality videos and illustrations.