4.2 Uveitis Differential Diagnosis and Aetiologies
Contents
There are several different descriptors that can be used to sensibly categorise intraocular inflammatory diseases [i]. The primary classification should be anatomical. By then describing a patient’s findings in with these additional terms and combining this classification with the demographics of the patient and relevant investigation findings, the differential diagnosis can be narrowed rapidly.
Jabs, D.A., Nussenblatt, R.B. and Rosenbaum, J.T. 2005. Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol 140(3) 509-516.
1. Anatomical
- Anterior uveitis
- Intermediate uveitis
- Posterior uveitis
- Panuveitis
2. Onset
- Sudden
- Insidious
3. Duration
- Acute (<3 months)
- Chronic (>3 months)
4. Course
- Acute (sudden onset, limited duration)
- Recurrent (repeated episodes with periods of inactivity off treatment)
- Chronic (repeated episodes requiring ongoing therapy)
ACUTE ( <3 months)
Idiopathic (30%)
Inflammatory
- HLAB27-associated – 50% (50% of these are seronegative spondyloarthropathies)
- Sarcoidosis
- Behcet’s disease
- VKH
- Sympathetic ophthalmia
- Sterile endophthalmitis (e.g. Post intravitreal Triamcinolone)
Infectious
- Viral (HSV, VZV or CMV) Fig. 4.2.3
- Syphilis
- Possner-Schlossman (?CMV)
- Associated with keratitis, scleritis or endophthlamitis (endogenous and exogenous)
Malignancies
- Lymphoma
- Melanoma
- Metastasis
Post-operative
- Retained lens fragment
- Chronic endophthalmitis
Traumatic
Lens-related
- Uveitis-Glaucoma-Hyphaema (UGH) Syndrome
- Phacoanaphylaxis
Anterior segment ischaemia
Drugs
- Rifabutin
- Cidofovir
- Bisphosphonates
Other
- Schwartz Syndrome (inflammation and raised IOP associated with chronic retinal detachment)
Chronic ( >3 months)
- All causes of acute uveitis can become chronic if untreated
- Fuch’s uveitis syndrome
- Juvenile Idiopathic Arthritis (JIA)
- TINU
Aetiologies from Clinical Features
Elevated IOP
- Possner Schlossman (?CMV)
- Sarcoidosis
- Herpetic (HSV, VZV)
- Toxoplasmosis
- Fuchs uveitis syndrome
- Lens induced
- Schwartz Syndrome
Granulomatous
- Sarcoidosis
- VKH
- TB
- Syphilis
- Sympathetic Ophthalmia
Hypopyon
- Seronegative spondyloarthropathies (HLAB27)
- Behçet’s disease (mobile hypopyon)
- Malignancy
- Rifabutin or cidofovir
- Endogenous or Exogenous Endophthalmitis
- Sterile Endophthalmitis (e.g. secondary to intravitreal Triamcinolone)
Aetiologies
- Idiopathic (80%)
i. Pars-planitis- presence of a “snow bank” (30%) - Inflammatory
i. Sarcoid
ii. Multiple sclerosis (MS)
iii. Inflammatory bowel disease (5% of IBD patients) - Malignancy
i. Lymphoma (primary CNS) (older age and usually NO CMO) - Infective
i. Tuberculosis
ii. Toxocara
iii. Syphilis
Investigations
- Form a differential diagnosis based on clinical examination, history and review of symptoms
- If there are suspicious neurological symptoms, order neuroimaging to exclude MS or lymphoma. An MRI is also needed if considering treatment with biological agents.
- Perform a diagnostic vitreous biopsy if required
- The main complications of intermediate uveitis are CMO and disc oedema. Assess for this at every visit with the visual acuity and an OCT.
Management
- After coming to a reasonable differential diagnosis and outlining your primary investigations, you will be expected to have a broad management plan and potentially tailor it to the individual patients’ circumstances.
- Treat the vision, not the inflammation. Cells in the vitreous do not cause the same complications as cells in the anterior chamber.
- Be sure to rule out syphilis and tuberculosis before treating with systemic steroids and comment on why you have selected your chosen treatment modality. i.e. for unilateral disease, start with topical or regional treatments prior to systemic options if the severity of the pathology allows.
- Medical
- Topical
- Periocular steroid (particularly for CMO)
- Intraocular steroid (if non-infectious)
- Triamcinolone 4mg / 0.1mL
- Dexamethasone intravitreal implant
- Systemic immunosuppression
- Corticosteroids
- Steroid-sparing agents
- Biological agents
Paediatrics
Children with intermediate uveitis present many challenges:
- Delayed presentation and poorer vision
- Difficult examination
- Risk of amblyopia
- Wider differential diagnosis
- Increased risk of complications including neovascularisation and haemorrhage
- Administration of periocular steroids or intravitreal treatment requires general anaesthetic
- Increased risk of steroid related IOP rise
- Growth stunting with systemic steroids
- Cataract formation
- Compliance
Features of Posterior Uveitis
- Retinitis (obscures vessels)
- Neuroretinitis (swollen disc and macular star)
- Retinal vasculitis (arteritis, phlebitis)
- Choroiditis (does not obscure vessels)
Aetiologies
The differential diagnosis of posterior uveitis is wide. A careful, broad history including a directed review of systems should be taken. Travel, pets, occupation, vaccinations, hobbies and sexual history are all relevant. Attempt to narrow down the diagnosis to an infection, inflammatory or an atypical cause, then proceed accordingly. Sight-threatening posterior uveitis requires immediate empirical treatment covering all reasonable elements of the differential. A vitreous biopsy is often required to confidently exclude infection in these cases.
Infections
Bacterial
- Exogenous (post-procedural) endophthamitis
i. Post-cataract surgery - Staph epidermidis ~ 70%, Staph aureus
ii. Chronic post cataract surgery (>6weeks post op) - P.Acnes, Staph.epidermidis, Candida
iii. Post-intravitreal injection - Streptococcus specicies (Staphylococcal species are having a relative emergence due to the widespread use of procedural face masks) - Endogenous endophthalmitis
i. Klebsiella pneumoniae in patients with liver abscesses - Syphilis
- Tuberculosis
- Bartonella henselae (cat-scratch disease)
Viral
- HSV, VZV (acute retinal necrosis)
- CMV
Fungal
- Endogenous endophthalmitis
i. Candida
ii. Aspergillus - Presumed ocular histioplasmosis (POHS)
- Cryptococcus
Protozoal
- Toxoplasma
Nematodes and Helminths
- Toxocariasis
- DUSN
- Onchocerciasis
Inflammatory conditions
- Sarcoid
- Behcets
- VKH
- Sympathetic ophthalmia
- Idiopathic chorioretinitis (“white dot syndromes”)
i. APMPPE, Serpiginous, “Ampiginous”
ii. MEWDS, PIC / MFC, AMN, AZOOR
iii. Birdshot
iv. IRVAN
Malignancy
- Lymphoma
- Metastasis
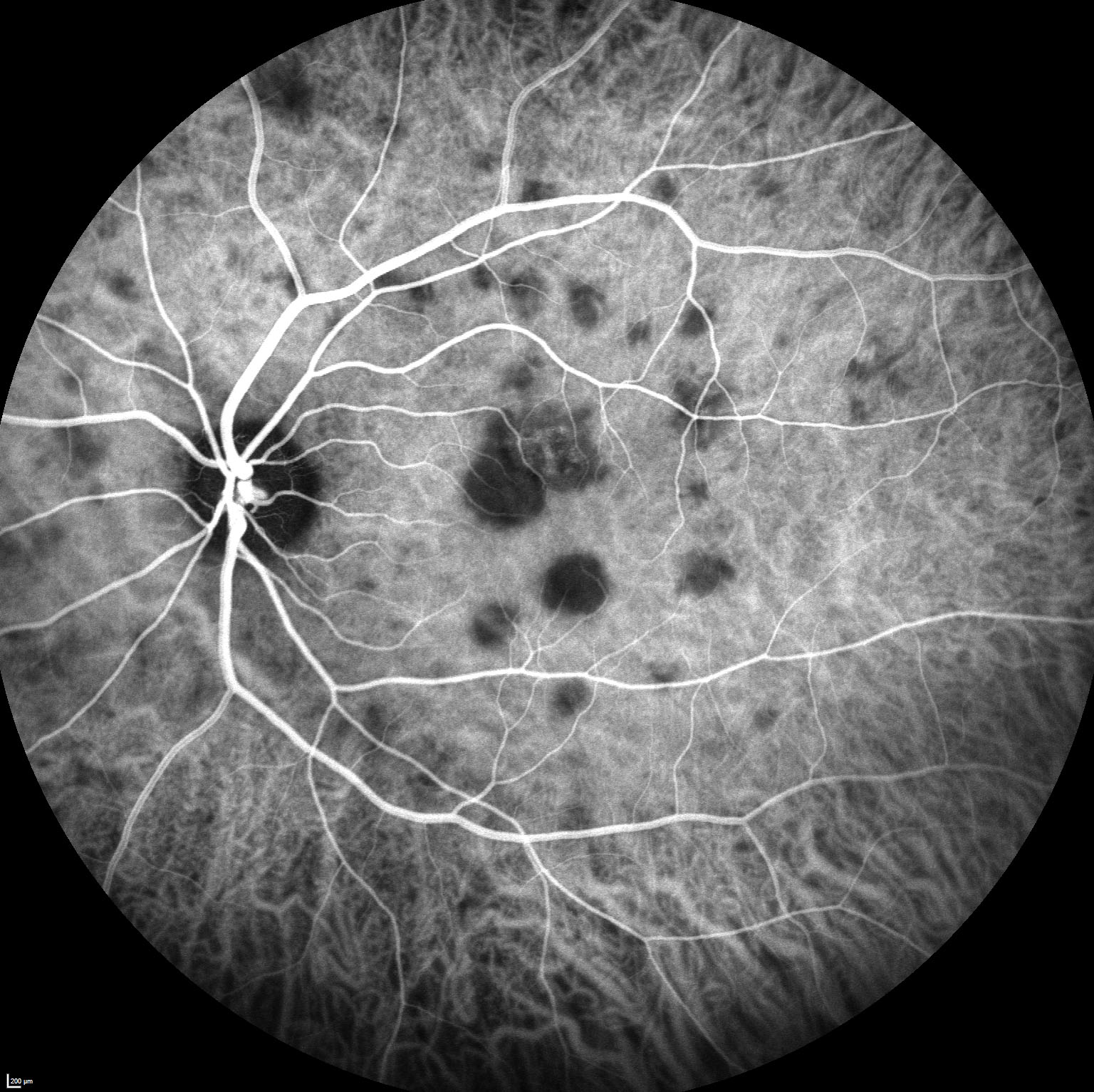
Retinal Vasculitis
Retinal vasculitis is important as secondary occlusions can develop. The differential diagnosis is narrowed considerably by careful observation of which vessels are inflamed [ii]:
Talat, L., Lightman, S. and Tomkins-Netzer, O. 2014. Ischemic Retinal Vasculitis and Its Management. Journal of Ophthalmology 2014 197675.
Arterial (Predominantly)
Venous (Periphlebitis)
Arterial (Predominantly)
Specific
Leads to ischaemia
Can be subtle when seen early (may need FFA to diagnose)
Venous (Periphlebitis)
Common, non- specific
May be ischaemic
Sheathing can persist post resolution of inflammation
Previous
4.1 Uveitis Examination
Next
5.1 Ectropion
All rights reserved. No part of this publication which includes all images and diagrams may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the authors, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law.
Vitreoretinal Surgery Online
This open-source textbook provides step-by-step instructions for the full spectrum of vitreoretinal surgical procedures. An international collaboration from over 90 authors worldwide, this text is rich in high quality videos and illustrations.