9 Investigations
9.1 Corneal Topography and Tomography
9.2 Confocal Microscopy
9.3 Optical Coherence Tomography - Macula
9.4 Optical Coherence Tomography Angiography (OCT-A)
9.5 Optical Coherence Tomography - Glaucoma
9.6 Optical Coherence Tomography – Anterior Segment
9.7 Fundus Autofluorescence Imaging
9.8 Fundus Angiography - Fluorescein
9.9 Fundus Angiography - Indocyanine Green
9.10 B-scan Ultrasonography & UBM
9.11 Electrophysiology
9.12 Automated Visual Fields
9.13 Neuroimaging
9.13 Neuroimaging
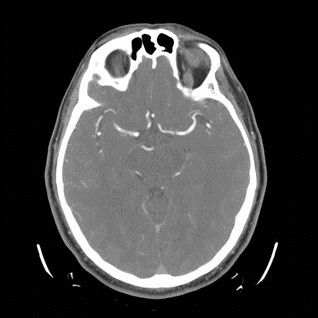
Computed Tomography (CT) uses ionising radiation (X-rays) to produce cross-sectional images. It is preferred over Magnetic Resonance Imaging (MRI) for acute haemorrhage, bone delineation, calcification and metallic foreign bodies. CT should be avoided in pregnancy. Communicating to the radiologist the purpose of the scan is essential for correct imaging and interpretation. CT scans of orbits/brain are often shown to examination candidates in conjunction with oculoplastic (e.g. orbital tumours) and neuro-ophthalmic (e.g. multiple sclerosis) cases. Candidates should have a basic understanding of how to describe a CT scan.
“This is a…
1. Axial/Coronal/Sagittal …
2. Orbital/Facial bones/Brain…
3. CT Scan…
4. of Name/Age/Date Taken”
- It is important that images be studied in more than one plane, otherwise pathology may be missed/misinterpreted
5. Bone (Brain Black) vs. Soft Tissue Windows
With bone windows, the brain is dark grey and bone is clearly delineated. With soft tissue windows the grey-white matter differentiation in the brain is clearly observed. Bone and soft tissue windows differ in two main ways:
- The window width and level used. Bone has a density of 300-3000 Hounsfeld units (HU). Soft tissue has a density of 30-50 Hounsfeld units (HU)
- The reconstruction algorithm. Bone windows use a sharp filter that enhances edges. The high resolution is optimal for bony detail, at the expense of increased noise (producing a grainy image). Soft tissue windows use a smoothing filter that reduces image noise at the expense of decreased spatial resolution
6. Contrast vs. Non contrast
- Contrast does not cross an intact blood brain barrier, and is therefore useful for suspected inflammation, infection and malignant processes when this barrier may be compromised. (Relative) contraindications of contrast include: allergy to iodine, renal failure, multiple myeloma, diabetes, severe cardiac disease, asthma and active thyroid orbitopathy. A standard post-contrast scan is a venous phase CT. CT angiography (CTA) can be performed to evaluate arteries
- Non-contrast CT can be used to evaluate haemorrhage, foreign bodies and orbital fractures
7. Normal (3mm) vs. Fine Slice
- Slices as fine as 1mm are useful for imaging optic canal trauma and foreign bodies and should be specifically requested. Most scanners now acquire volumetric information and fine slices can be requested post-scan if required
Adjectives: Hyper/hypodense
- Tissue density is represented on a grey-scale ranging from white (maximum, e.g. bone) to black (minimum, e.g. air)
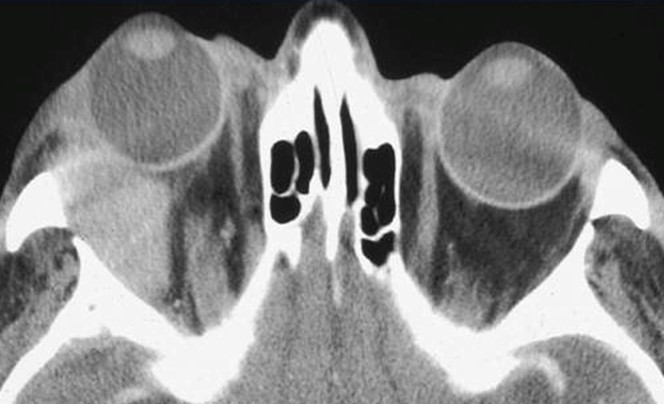
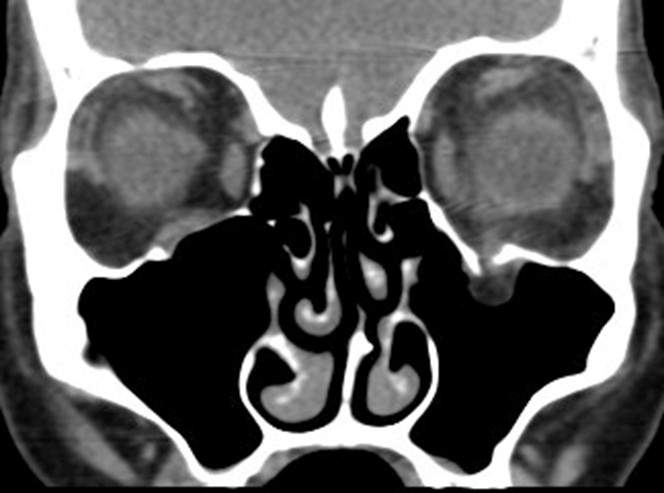
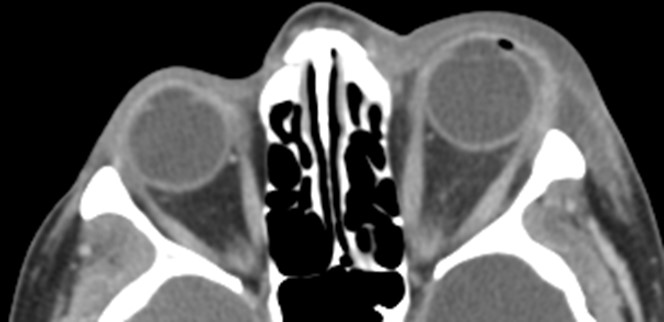
Figure 9.13.1 CT Bone vs Soft Tissue Windows
Coronal and axial views shown
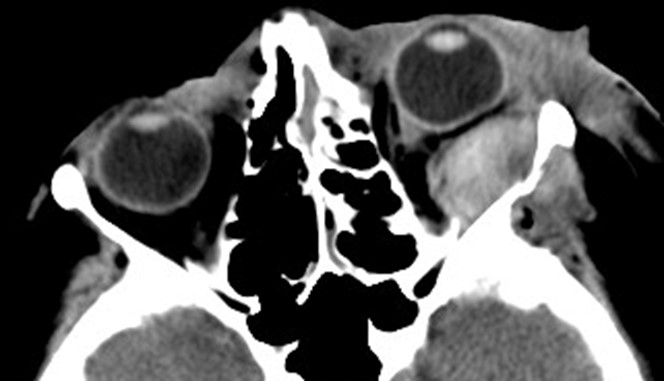
Figure 9.13.2
Non-contrast vs Contrast CT
Note that the superior ophthalmic veins highlight in the contrast CT.
- Figure 9.13.4: Blowout Fracture
- Figure 9.13.5: Cavernous Haemangioma (Orbital)
- Figure 9.13.6: Cellulitis – Post Septal (Orbital)
- Figure 9.13.7: Cellulitis – Pre Septal
- Figure 9.13.8: Hydrocephalus
- Figure 9.13.9: Idiopathic Orbital Inflammatory Disease
- Figure 9.13.10: Mucocele (Orbital)
- Figure 9.13.11: Pleomorphic Adenoma of the Lacrimal Gland
- Figure 9.13.12: Retrobulbar Haemorrhage
- Figure 9.13.13: Ruptured Globe
- Figure 9.13.14: Thyroid Orbitopathy
CT orbits is the neuro-imaging modality of choice for most patients with thyroid orbitopathy. Signs that may be present include:
- Enlargement of the extra-ocular muscles with tendon sparing (if non-tendon sparing consider other orbital inflammatory processes.
- Proptosis (approximately >1/3 of orbit anterior to line through lateral orbital rims)
- Increased orbital fat
Look at the orbital apex (coronal sections) for evidence of optic nerve compression Look at the bones/sinuses for orbital decompression
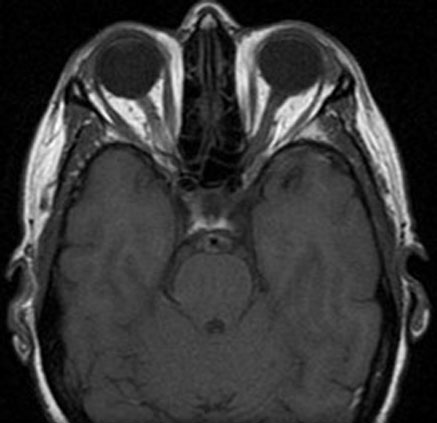
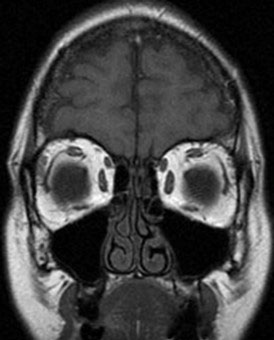
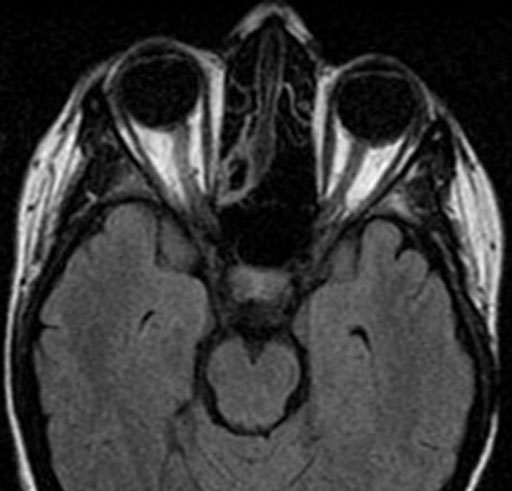
Magnetic Resonance Imaging (MRI) uses a large magnetic field to re-arrange protons in water molecules. The energy released by these protons re-equilibrating is then detected by a scanner to generate an image. MRI is preferred over Computed Tomography (CT) for soft tissue visualisation, demyelination and infarction. MRI is contraindicated with metallic foreign bodies and implants. Communicating to the radiologist the purpose of the scan is essential for correct imaging and interpretation. MRI scans of orbits/brain are often shown to examination candidates in conjunction with neuro-ophthalmic cases. Candidates should have a basic understanding of how to describe a MRI scan.
“This is a…
1. Axial/Coronal/Sagittal …
2. Orbital/Brain…
3. MRI scan…
4. of Name/Age/Date Taken”
- It is important that images be studied in more than one plane, otherwise pathology may be missed/misinterpreted
5. T1 or T2 Weighted
- Most images are a mix of T1 or T2, but weighted towards one
6. Fat Saturated/Suppressed
7. Gadolinium Enhanced
8. FLAIR
9. DWI
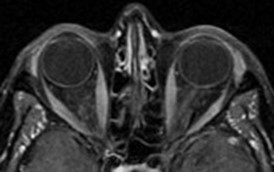
A Typical MRI Orbit Protocol Includes:
Whole Brain
- T1 (Axial)
- T1 (Sagittal)
Orbits
- T1 (Axial)
- T1 (Coronal)
- T1 Fat saturated with gadolinium (Axial)
- T1 Fat saturated with gadolinium (Coronal)
- T2 Fat saturated (Coronal)
- T1 fat saturated, gadolinium enhanced MRI’s are most commonly used for orbital pathology. Additional sequences can be performed according to the pathology being evaluated
Adjectives: Hyper/hypointense
- Intensity depends on the water content of structures and the magnetic relaxation properties of protons in different tissues
T1 Weighted
T2 Weighted
Water (CSF, vitreous, oedema)
T1 Weighted
Black
T2 Weighted
White
(“Tea for two”- milk is white!)
Fat, blood, contrast
T1 Weighted
White
T2 Weighted
Variable
T1 Weighted
Grey matter (superficial) is darker
White matter (deep) is lighter
T2 Weighted
Grey matter (superficial) is lighter
White matter (deep) is darker
Best For
T1 Weighted
Anatomic detail
T2 Weighted
Pathology
T1 Weighted
T2 Weighted

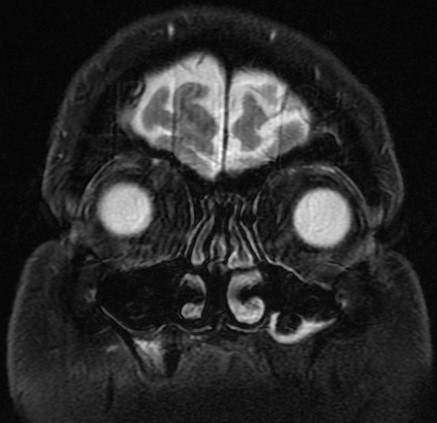
Fat saturated/suppressed
(More commonly T1)
FLAIR (Fluid Attenuated Inversion Recovery)
Fat saturated/suppressed
(More commonly T1)
Suppresses white fat signal (fat is now black).
FLAIR (Fluid Attenuated Inversion Recovery)
Suppresses fluid (CSF and vitreous are black).
Compared with T1, FLAIR images are sharper but have more “noise”.
Look for white rim at anterior border of lateral ventricles.
White is abnormal.
Best For
Fat saturated/suppressed
(More commonly T1)
Recommended for all orbital MRI.
Improved view of: optic nerve, extra-ocular muscles, lacrimal gland, tumours, inflammatory lesions, vascular malformations.
FLAIR (Fluid Attenuated Inversion Recovery)
Demyelinating disease.
Oedema.
Fat saturated/suppressed
(More commonly T1)
.jpg)
FLAIR (Fluid Attenuated Inversion Recovery)
Gadolinium
(Always T1, usually fat saturated)
White: extra-ocular muscles, venous sinuses.
Best For
Tumours, inflammatory lesions
Remains intravascular unless there is a break-down in the blood brain barrier.
Previous
9.12 Automated Visual Fields
Next
10.1 Lensmeter
All rights reserved. No part of this publication which includes all images and diagrams may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the authors, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law.
Vitreoretinal Surgery Online
This open-source textbook provides step-by-step instructions for the full spectrum of vitreoretinal surgical procedures. An international collaboration from over 90 authors worldwide, this text is rich in high quality videos and illustrations.
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
-(Pre-Contrast).jpg)
-(Post-Contrast).jpg)
.jpg)


.jpg)