7 Neuro-Ophthalmology
7.1 Cranial Nerve III (Oculomotor) Palsy
7.2 Cranial Nerve IV (Trochlear) Palsy
7.3 Cranial Nerve VI (Abducens) Palsy
7.4 Cranial Nerve VII (Facial) Palsy
7.5 Optic Nerve Function
7.6 Visual Fields to Confrontation
7.7 Pupils
7.8 Horner’s Syndrome
7.9 Nystagmus
7.10 Neuro-Ophthalmic Differential Diagnoses and Aetiologies
7.6 Visual Fields to Confrontation
Visual fields to confrontation are often tested in examinations. If performed systematically and the patient’s fixation is controlled, the location of the defect can usually be determined rapidly. Candidates can then proceed to look for additional signs consistent with that lesion. Common field defects in examinations include homonymous hemianopias, quadrantanopias and bitemporal hemianopias.
- Have a diffuse overhead light
- Sit directly in front of the patient, at their level
- Sit with your knees nearly touching their knees, that helps you determine the halfway point when holding a visual target
- Shake their hand to determine if they are right or left-handed
- Ask for this. If not provided, check that the patient can count fingers (CF) in each eye (if they can’t, visual fields will be meaningless)
- Ask the patient to look at your nose, then ask them “Can you see my whole face”? “Is any of it missing?” Inability of the patient to see one side or a quarter of your face may allow you to quickly identify a homonymous hemianopia or quadrantanopia
- Ask the patient to “Cover this eye (point to their left eye) with your left hand (ensure the patient properly covers their eye with their palm to avoid cheating through their fingers) and look at my open eye”. When sitting directly in front of the patient, close your eye that is directly opposite their covered eye. This way they can look into your open eye. It is crucial that the patient fixes on your open eye throughout the test (continuously check that they do not look directly at your fingers), otherwise the test is invalid. For some patients this often requires repeat prompting! Ask the patient to “Use your peripheral vision to tell me how many fingers I’m holding up”
Check for a Scotoma
- Present the fingers of your left hand (1, 2 or 5) in each of 4 quadrants and get the patient to count them aloud. Ensure that you present your fingers midway between yourself and the patient (this takes practise). Repeat for the other eye
Map Out Any Scotoma(s)
- If the patient has a scotoma, it needs to be mapped out
Remember:
- Neurological fields tend to respect the vertical meridian
- Glaucomatous fields tend to respect the horizontal meridian
- Always map out scotomas in the direction from non-seeing → seeing. Do this slowly enough that the patient can register a change
- Mapping of scotomas can be done with a moving finger, red hat pin or red top (atropine) bottle. If there is an obvious meridional defect, this meridian should be tested first. Otherwise, test from the periphery → centre
- The presence of a relative scotoma (in which a patient can see but less well than in the non-scotomatous region) can be checked by asking the patient to compare red saturation across meridians using 2 red top (atropine) bottles. Ensure that your red-top bottles are the same redness! Test by holding one red top bottle on either side of the vertical midline, first above then below the horizontal. Then test with one red top bottle on either side of the horizontal midline, first left of the vertical midline, then right
- Repeat for the other eye
- This will not need to be routinely tested but should be considered if the patient is known to have optic nerve pathology (such as disc swelling)
- Ask the patient to focus on a red hat pin presented directly in front of their eye. Move a hat pin of a different colour (or white cotton swab) temporally until they lose sight of it. Ensure these are midway between yourself and the patient so that you are checking your blind spot and comparing it to theirs at the same time
- Again this will not need to be routinely tested, but should be considered if the patient is known to have a parietal lobe lesion. Most commonly there is involvement of the right parietal lobe, affecting the left side of space. After ensuring that the patient can count fingers with each eye individually, have them open both eyes. Hold up 3 of your fingers (2 on one hand and 1 on the other) and ask them to count the total number of fingers. Alternate the number and combination of fingers. Inability to count one side when both sets of fingers are presented simultaneously indicates visual neglect of that side
Summary
- Right or left (or binocular / homonymous)
- Absolute or relative
- Congruent or incongruent
- Hemianopia, quadrantanopia etc.
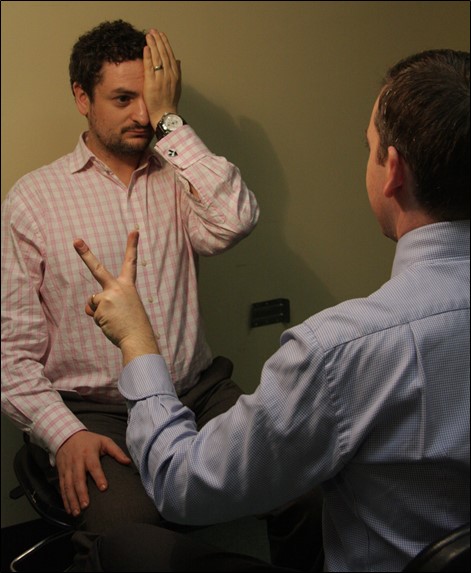
Figure 7.6.1
Testing Visual Fields to Confrontation in the Inferotemporal Quadrant
The examiner is at the same level as the patient and has his fingers equidistant between the patient and himself. The patient is fixing on the examiner’s left eye with his right eye and has his left eye fully covered by his palm.
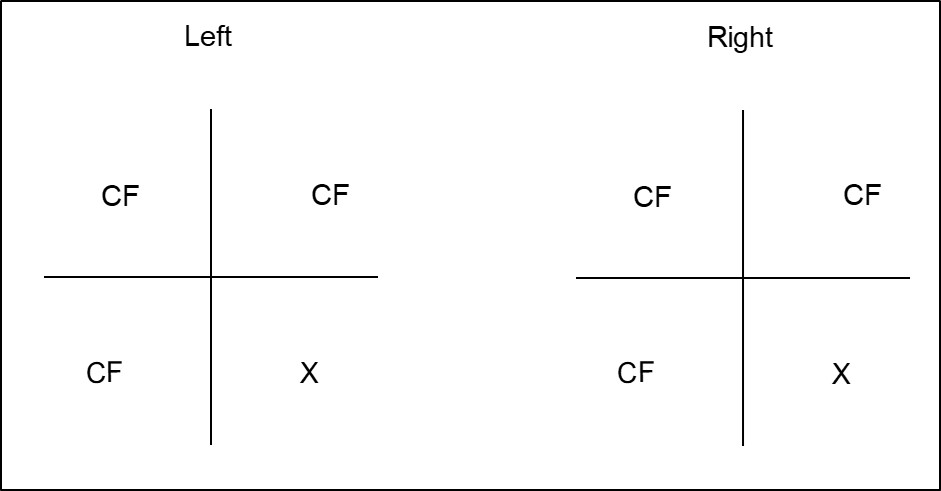
Figure 7.6.2
Documenting Visual Field Defects
Visual field defects should be documented from the patient’s perspective, but it is advisable to label the eyes. If extra clarification is required, the sides of the visual field (nasal / temporal) can be documented to avoid confusion. Alternatively one can describe the type of visual field defect (e.g. “left homonymous hemianopia”).
- Further examination is directed by the type of field defect diagnosed
1. Homonymous Hemianopia / Quadrantanopia
- The lesion is in the contralateral cerebral hemisphere, anywhere from the lateral geniculate nucleus via the optic radiations to the occipital (visual) cortex. Anterior optic radiation defects give more incongruent field defects. Temporal lobe lesions are uncommon
- Check for optokinetic nystagmus (OKN) asymmetry:
- Move the tape towards the side of the lesion (i.e. In a left homonymous hemianopia affecting the right cerebral hemisphere, move the tape to the patient’s right)
- Deep Parietal lesions
- OKN slower / poorer when moving the tape towards the lesion (since pursuit movements are generated here)
- Occipital lesions
- OKN symmetrical both ways
- Check for hemiplegia
- Check for other parietal lobe signs (see below)
2. Bitemporal Hemianopia
Does the patient have a craniotomy scar or look acromegalic?
- Check for red desaturation across the vertical midline, RAPD
- Check for cranial nerve palsies (involvement of cavernous sinus)
- Examine the optic nerve (for optic disc swelling or atrophy ± bowtie)
3. Constricted Visual Fields
- Retinitis pigmentosa, advanced glaucoma etc.
4. Central Scotoma
- Macular disease, optic atrophy etc.
5. Enlarged Blind Spot
- Optic disc swelling
For patients who are right-handed, the dominant hemisphere is the left 90% of the time. For patients who are left-handed, dominance of hemispheres is 50% either side.
Features
Clinical Tests
Dominant
(Usually Left)
Gerstmann’s syndrome:
Acalculia
Impaired serial 7’s
Agraphia
Impaired writing
Left-right disorientation
Can’t show you L and R hand or touch L ear with R hand
Finger agnosia
Can’t name their fingers
Previous
7.5 Optic Nerve Function
Next
7.7 Pupils
All rights reserved. No part of this publication which includes all images and diagrams may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the authors, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law.
Vitreoretinal Surgery Online
This open-source textbook provides step-by-step instructions for the full spectrum of vitreoretinal surgical procedures. An international collaboration from over 90 authors worldwide, this text is rich in high quality videos and illustrations.
