5.4 Ptosis
Introductory Comments
In clinical examinations, a patient with (blepharo)ptosis may present in two different ways. Firstly, as a neuro-ophthalmic diagnostic dilemma (particularly neurogenic and myogenic ptosis); secondly, as an oculoplastic management dilemma (particularly aponeurotic and mechanical ptosis). The candidate must be aware of this and be able to simultaneously consider diagnosis and management options.
The ptosis examination is extremely important as some systemic conditions that present with ptosis are potentially life threatening. These include: Myasthenia Gravis, Chronic Progressive External Ophthalmoplegia (CPEO), Horner’s syndrome and pupil-involving CNIII palsy.
Amblyopia may occur following congenital ptosis. A ptotic lid can induce astigmatism and reduce the BCVA.
- Always shake the patient’s hand with a firm grip
- A grip that is slow to release is suggestive of Myotonic Dystrophy
- General appearance / speech (Myasthenia Gravis, Myotonic dystrophy, CPEO, CN III palsy)
- Walking aids, slurred or nasal speech and mask-like facies may suggest a neuromuscular disorder
- Patients may adopt a chin up posture or exhibit brow overaction to compensate for the ptosis
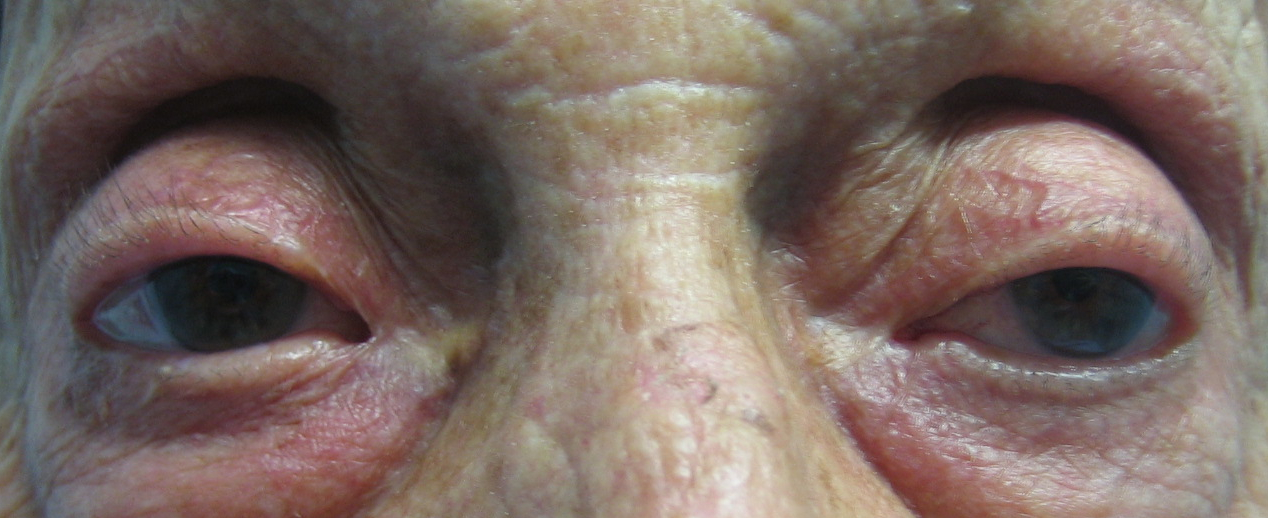
- Upper eyelid / Ptosis (partial vs. complete ptosis; unilateral vs. bilateral ptosis)
- Does it cross the visual axis (especially in a child)?
- Chin-up head posture, brow over-action (compensatory)
- Dermatochalasis, brow ptosis
- Absent or high lid crease; Deep upper lid sulcus (aponeurotic ptosis).
- Strabismus (CN III palsy, myogenic causes of ptosis)
- Pupils (anisocoria) (Horner’s syndrome, CN III palsy)
- If anisocoria is present, measure the pupil size in light and dark to confirm which pupil is abnormal. Anisocoria should direct you towards finding a potentially life-threatening neurological cause (Horner’s Syndrome or CN III palsy)
- Heterochromia iridis (Congenital or early acquired Horner’s Syndrome)
- Proptosis or enophthalmos (measure or request Hertel exophthalmometry)
- Other features: reverse ptosis, anhidrosis
Differentiating an Aponeurotic Ptosis from a Congenital Ptosis
± Ask the patient to “Look down at my finger” (hold this below primary). The affected upper eyelid may be:
- Lower than the contralateral side (aponeurotic ptosis)
- Higher (“hang-up”) than the contralateral side (simple congenital ptosis)
Congenital ptosis lids will generally have a poorly defined or absent skin crease. Aponeurotic ptosis lids will have deep sulci and a high skin crease. Congenital ptosis may also be associated with monocular elevation palsy or Marcus Gunn jaw-winking syndrome.
Assess for a Marcus Gunn Jaw-Winking Syndrome
± Ask the patient (especially children) to “Please open your mouth / move your jaw side to side / eat / suck a straw”. Patients with Marcus Gunn Jaw-Winking Syndrome will demonstrate dynamic elevation of the ptotic lid.
Figure 5.4.2
Marcus Gunn Jaw-Winking Syndrome
- These are important in determining the cause and management of a ptosis but are less important under examination conditions if the ptosis is thought to be neurological.
- Levator function is the most important measurement to determine what type of surgery will be performed
- Holding a pen torch in your right hand and a ruler vertically in the left… ask the patient to:
Instruction
“Look at the torch”
(held in primary)
Measurement
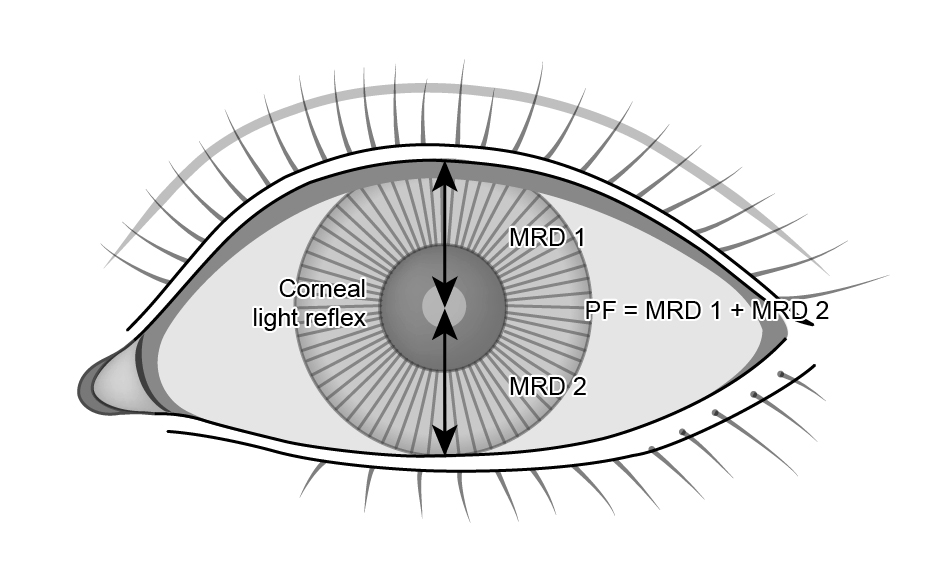
Palpebral Fissure (PF)
Distance between the upper and lower eyelid margins in the pupillary plane.
Normal
8mm (M), 10mm (F)
Marginal Reflex Distance 1 (MRD1)
Distance from upper eyelid margin to corneal reflex.
Normal ~ 4mm
< 2mm = “ptosis”
Instruction
“Look all the way down”
Measurement
Upper Lid Crease (LC)
Distance from the upper eyelid margin (in downgaze) to most prominent crease.
Normal
Normal = 8mm (M), 10mm (F)
(absent / high = aponeurotic)
“I’m going to press quite firmly here” (put torch down, stabilise brow / frontalis muscle with your left hand)
Instruction
“Look all the way up”
Measurement
Levator Function (LF)
Distance that the upper eyelid margin travels in excursion from down to upgaze. The action of the brow must be stabilised.
Normal
≥ 15mm Normal
<10mm Poor
< 5mm Very poor (likely myogenic ptosis, congenital ptosis, CNIII palsy)
Manually elevate the ptotic eyelid to see if the contralateral side falls (Herrings law). This is known as “enhanced ptosis” and suggests the presence of bilateral (masked) ptosis. An alternative is to use 10% phenylephrine drops in the ptotic eye to stimulate Muller’s muscle. Masked ptosis in the contralateral eye will be revealed as the ptotic lid elevates
Under exam conditions there is rarely sufficient time to perform cover testing. Proceed to examining ocular rotations with an “H” pattern. Potential causes of ptosis and eye movement disorders include: CNIII palsy, Myasthenia Gravis, Chronic Progressive External Ophthalmoplegia (CPEO), Oculopharyngeal dystrophy, Myotonic dystrophy, Monocular elevation deficit (pseudo-ptosis)
Check for: - Aberrant regeneration (CN III palsy) - Elevation defect (superior rectus weakness in congenital ptosis) - Saccades (slow, hypometric and “glissadic” (gliding) saccades may occur in many neurogenic / myogenic conditions such as Myasthenia gravis and CPEO)
i. Cogan’s Lid Twitch
Hold your finger horizontally in the patient’s downgaze and ask them to look at this for several seconds. Hold a pen horizontally in the patient’s primary gaze and ask them to “Look at the pen”. Look for twitch of the upper eyelid on saccade from downgaze to primary. Sometimes the upper eyelid will overshoot, then gradually fall (become more ptotic) - this is also abnormal.
ii. Fatigueability
Hold a pen horizontally in the patient’s upgaze and ask them to “Look at the pen”. Say aloud (to the examiner) “I am looking for fatigueability” (worsening ptosis). As there is usually insufficient time in examinations (ideally the upgaze should be held for 2 minutes), the examiner will often disclose any potential fatigueability to the candidate and ask them to proceed with the rest of the examination.
iii. Orbicularis Oculi
Starting with the patient’s eyes open, use your thumb and index finger of both hands to hold open the upper and lower eyelids of both of the patient’s eyes. Ask the patient to “Close your eyes as hard as you can”. Inability by the patient to overcome your grip and close his / her eyes is suggestive of neuromuscular disease such as Myasthenia Gravis.
Eyelid closure may be reduced in neuromuscular disorders. It is also essential to test this as any surgical intervention may risk of corneal exposure. See Section 5.1.6 Corneal Exposure Risk.
- Evert the upper eyelid for a mechanical cause (especially if unilateral ptosis)
- Slit-lamp examination
i. Look for evidence of exposure (with fluorescein staining)
ii. Look for pigmentary retinopathy (Kearns-Sayre syndrome) - Bulbar musculature
i. Ask patient to say “123456789”, “ppp” (CNVII), “kkk” (CNX), “ttt” (CNXII)
ii. Speech may be affected in Myasthenia Gravis, CPEO, Oculopharyngeal dystrophies and Myotonic Dystrophy
iii. Look for facial synkinesis following CN VII palsy - Other signs of Horner’s Syndrome (see Section 7.8)
- Check old photos (particularly for suspected congenital ptosis)
- Check pulse, ECG i. Kearns-Sayre syndrome (look for heart block)
- Ice test i. Place covered ice over eyelids for 2 minutes. A 2mm improvement in ptosis after 2 minutes is very sensitive and specific for Myasthenia Gravis.
- Phenylephrine 10% test
i. Stimulate Muller’s muscle (consider in mild ptosis)
ii. Beware of cardiac complications of this test
Summary
- Right or left (unilateral or bilateral)
- Involutional / myogenic / neurogenic / mechanical ptosis
- ± Good / poor levator function
- ± Corneal exposure
- Paediatric ptosis: Check for occlusion amblyopia, jaw-wink, levator function
Inspection
± Chin up position, Brow over-action?
Symmetry
Aponeurotic
Bilateral (but asymmetrical)
Neuromuscular junction (Myogenic)
Bilateral
Neurogenic
Unilateral
Mechanical
Unilateral
Congenital
Unilateral (most)
Lid features
Aponeurotic
Deep sulci,
Lids low on downgaze
Congenital
Lid high on downgaze (congenital) [ii]
± Jaw-wink
Poor relaxation of the levator.
Superior Lid Crease
Aponeurotic
Absent / high (>12mm) [iii]
Neuromuscular junction (Myogenic)
Variable
Neurogenic
Normal
Mechanical
Variable
Congenital
Shallow / absent
If the posterior attachments of the levator aponeurosis to the tarsus detach but the anterior attachments to the skin remain intact, pulling the skin crease superiorly.
Levator Function
Aponeurotic
Normal or only slightly reduced
Neuromuscular junction (Myogenic)
Decreased
Neurogenic
Variable (normal in Horner’s Syndrome)
Mechanical
Variable
Congenital
Decreased
Pupils
Neurogenic
Miosis (Horner’s)
± Mydriasis (CNIII palsy)
Eye movements
Neuromuscular junction (Myogenic)
Often affected
Slowed Saccades
Neurogenic
Features of CNIII palsy
Congenital
May have upgaze (superior rectus) deficit
Typical management
Aponeurotic
Levator advancement /
plication or resection
Neuromuscular junction (Myogenic)
Investigate / manage underlying disease
Rule out Kearn-Sayre Syndrome
Neurogenic
Rule out life-threatening causes
Correct strabismus prior to ptosis
Mechanical
Removal of the mass
Congenital
Brow suspension if adequate frontalis action
Investigations are dictated by the provisional cause for the ptosis. Investigations that may be required include:
- Orbital Imaging (particularly if proptosis or enophthalmos are present)
- Myasthenia Gravis
- Antibodies
- ACh receptor (“Binding” type in 50% of ocular MG, 90% generalized MG, Specific)
- ± Anti-MuSK (muscle specific kinase) (in 20% of AChR negative MG but rare in ocular MG)
- ACh receptor (“Binding” type in 50% of ocular MG, 90% generalized MG, Specific)
- Tensilon (edrophonium)
- Give 2mg (2mL) IV (test dose, wait 2mins)
- Give 8mg (8mL) IV (actual dose)
- There is a risk of a cardiovascular arrest. Ensure IV Atropine resuscitation equipment available
- Longer-acting, useful in children
- Give 2mg (2mL) IV (test dose, wait 2mins)
- Single fibre EMG
- Gold standard (99% sensitive) but not very useful in purely ocular myasthenia.
- CT chest with contrast
- Thymomas are present in 15% of patients with myasthenia gravis
- TFTs and TRAB
- Association with autoimmune disease and especially Grave’s disease
- Antibodies
- Mitochondrial myopathies (including CPEO, Kearns-Sayre syndrome)
- ⊕ Muscle biopsy (deltoid)
- Ragged red muscle fibres represents accumulation of abnormal mitochondria
- Serum lactate / CK / glucose
- ↑ CSF protein
- (-) ACh receptor antibodies, (-) Tensilon
- Cardiovascular work up for heart block in Kearn-Sayre Syndrome
- Ragged red muscle fibres represents accumulation of abnormal mitochondria
- ⊕ Muscle biopsy (deltoid)
Previous
5.3 Eyelid Tumours
Next
5.5 Orbit
All rights reserved. No part of this publication which includes all images and diagrams may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the authors, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law.
Vitreoretinal Surgery Online
This open-source textbook provides step-by-step instructions for the full spectrum of vitreoretinal surgical procedures. An international collaboration from over 90 authors worldwide, this text is rich in high quality videos and illustrations.